Session Information
Date: Saturday, October 6, 2018
Session Title: Clinical Trials and Therapy in Movement Disorders
Session Time: 1:45pm-3:15pm
Location: Hall 3FG
Objective: The primary objective of this observational study was to evaluate the proportion of Parkinson’s disease (PD) patients identified as advanced PD (APD) patients according to physician’s judgment in four participating movement disorder centers (MDC) across the study.
Background: APD therapies are typically provided at MDCs by a multidisciplinary expert team. Yet, lack of universally accepted APD diagnosis, treatment criteria or guidelines, render it difficult to appropriately allocate resources and refer patients to device aided treatment (DAT) in a timely manner.
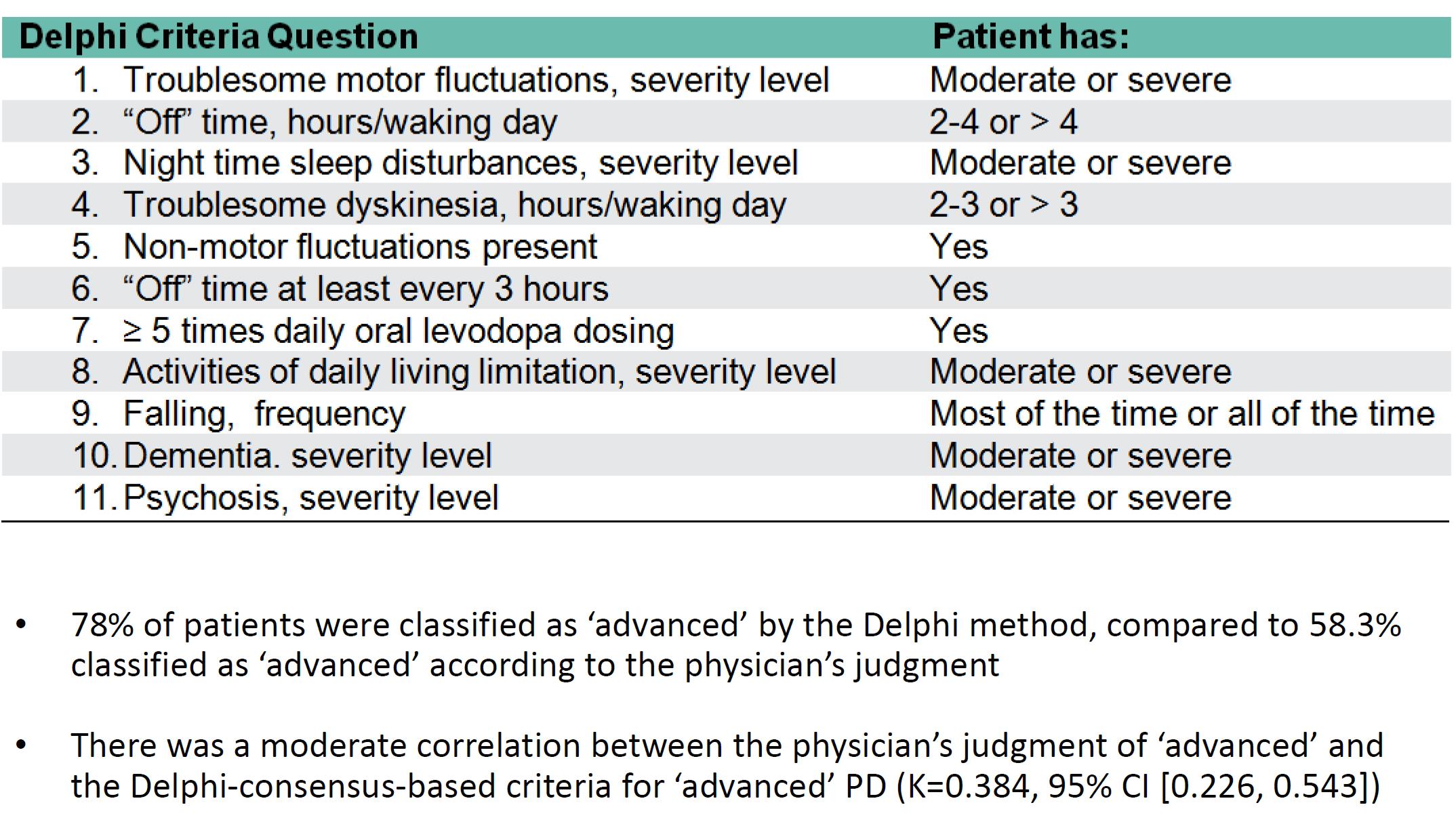
Methods: In a multi-country, cross-sectional study, PD patients undergoing routine outpatient evaluation or inpatients at one of 4 Israeli MDCs, were evaluated based on both the physician’s judgment and the Delphi consensus criteria2. The percentage and profile of APD patients identified by physician judgement versus the Delphi method were compared. A sub analysis of data collected from patients in these Israeli MDCs is presented.
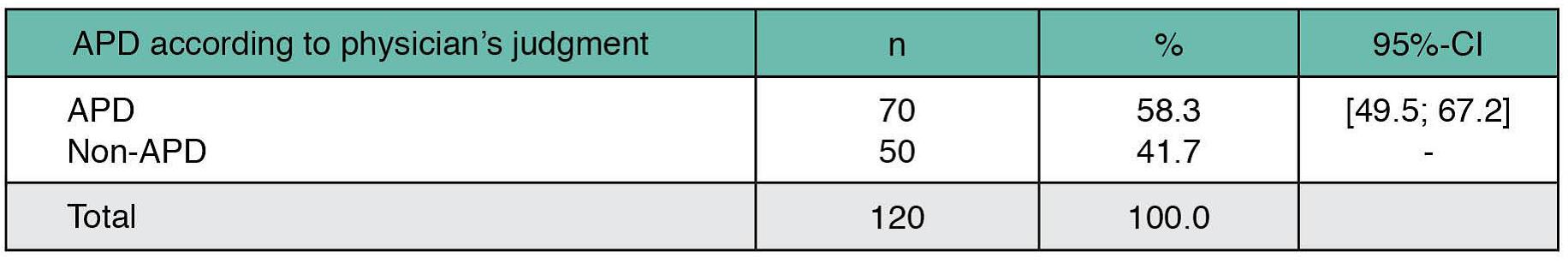
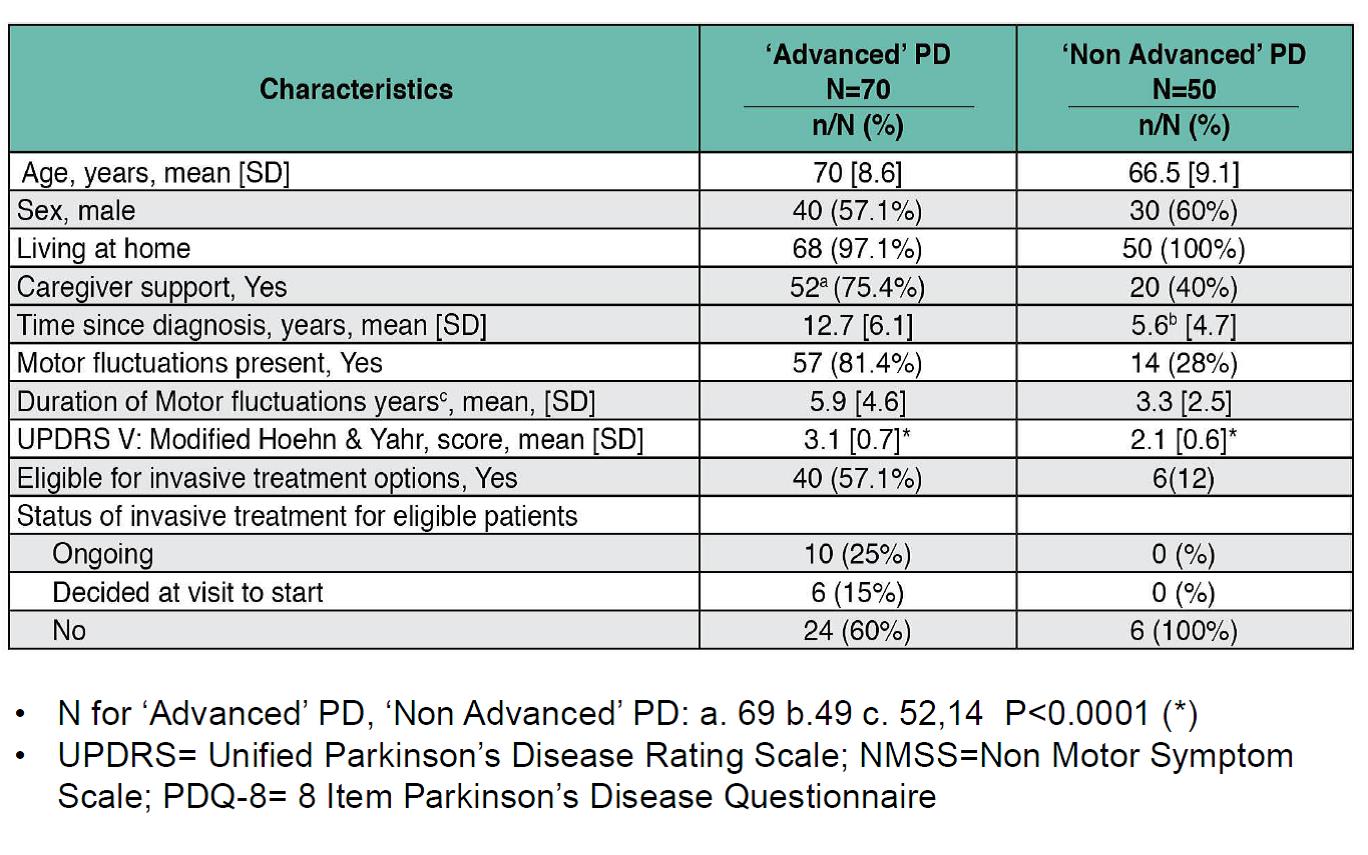
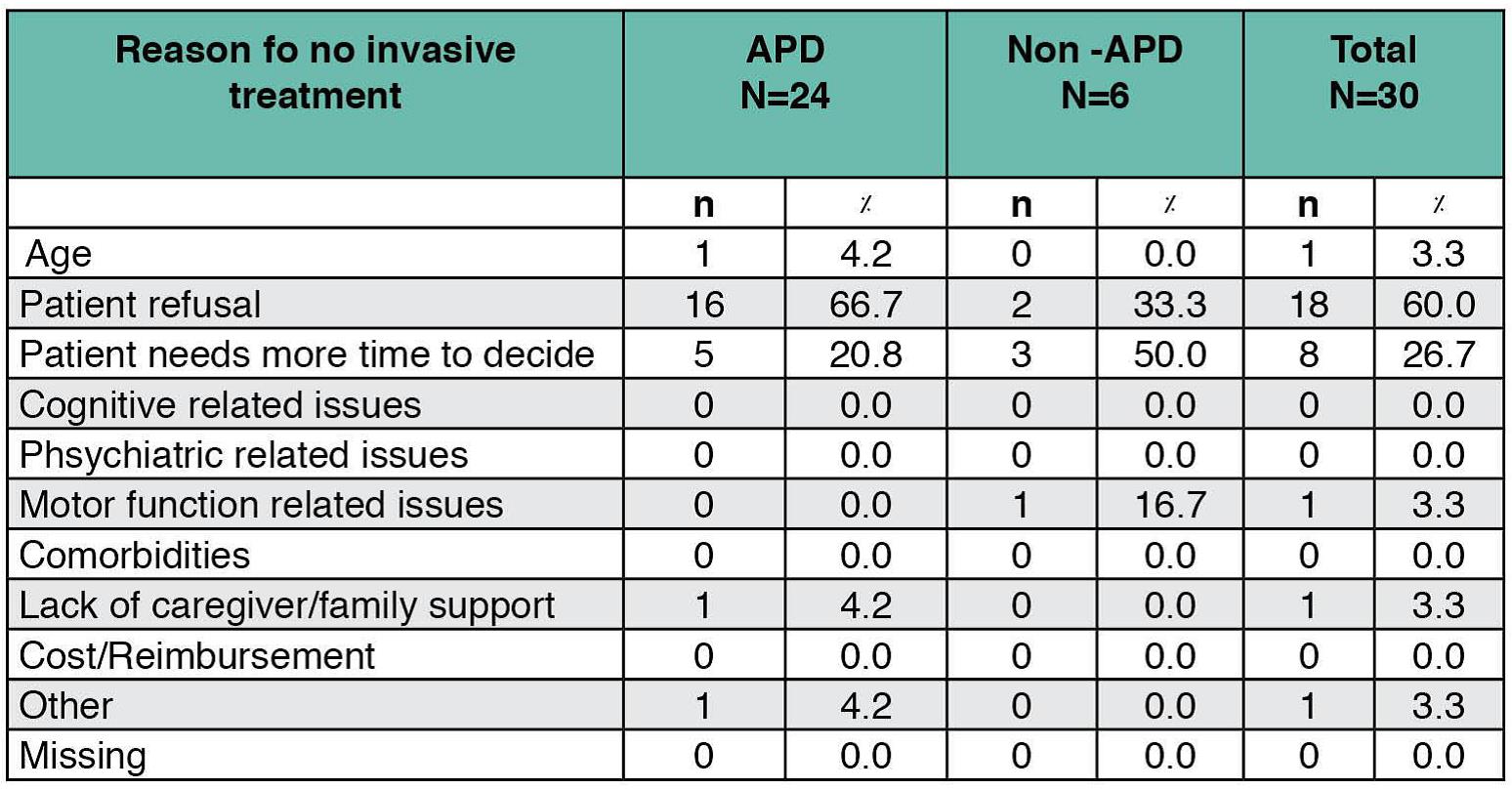
Results: The 120 patients evaluated were registered as patients at one of 4 MDCs in Israel for a mean of 5.4 years since referral, with the majority referred to the center by a neurologist (65.8%). Physician assessments categorized 58.3% of patients as APD [table1], 81.4% of whom presented motor fluctuations and with a mean of 12.7 years following diagnosis [table2]. In contrast, 28% of the non-APD patients presented motor fluctuations and were within an average 5.6 years following diagnosis. While DAT was recommended for 57.1% of APD patients, versus 12% of non-APD patients, no such treatment was either ongoing or planned for 60% of eligible APD candidates [table2]. Treatment type for patients on ongoing DAT included neurosurgery (n=5) and levodopa-carbidopa intestinal gel (n=5). The main reason for no current DAT in eligible APD patients was mainly due to patient refusal (66.7%) [table3]. The highest agreement in classifying a patient as APD between physician judgment and Delphi classification was in assessments of activities of daily living, daily OFF hours and motor fluctuations [table4].
Conclusions: Physician’s judgment in classifying APD correlated with select Delphi criteria. Yet, even in cases of physician agreement with APD classification, initiation of DAT was not accomplished mainly due to patient refusal.
References: 1-Djaldetti et al Israeli Annual Neurology Congress 2017. 2-Antonini A. Implementing a Delphi Panel to Improve Understanding of Patient Characteristics of Advanced Parkinson’s Disease. Poster presented at: 19th International Congress of Parkinson’s disease and Movement Disorders; June 14–18, 2015; San Diego, CA, USA.
To cite this abstract in AMA style:
R. Djaldetti, S. Hassin-Baer, M. Anca-Herschkovitsch, R. Gross, R. Cohen, H. Banayan, K. Onuk, T. Gurevich. Advanced Parkinson’s disease Diagnosis and Treatment Trends in Israel – Sub-Analysis of the OBSERVE-PD Multi-Country, Cross-Sectional Study [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/advanced-parkinsons-disease-diagnosis-and-treatment-trends-in-israel-sub-analysis-of-the-observe-pd-multi-country-cross-sectional-study/. Accessed November 16, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/advanced-parkinsons-disease-diagnosis-and-treatment-trends-in-israel-sub-analysis-of-the-observe-pd-multi-country-cross-sectional-study/