Session Information
Date: Wednesday, September 25, 2019
Session Title: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Agora 3 West, Level 3
Objective: This study aims to explore the relationship between pain and other non-motor symptoms in Parkinson Disease (PD).
Background: Pain is a common non-motor symptom (NMS) in PD that is difficult to treat.[1-3] Evidence suggests that impaired central nociceptive processing plays a role in the pathogenesis of pain in PD.[3] Furthermore, pain may cluster with other NMS like sleep disturbance, autonomic dysfunction and depression, possibly implicating a common pathophysiology.[4,5] Adequate treatment of pain may require treating related NMS.
Method: This is a cross-sectional, observational study of consecutive patients with idiopathic PD, ages 18-85. Subjects were evaluated at two academic centers using the UPDRS III, King’s PD Pain Scale (KPPS), Non-Motor Symptoms Scale (NMSS) and Beck Depression Inventory (BDI). Exclusion criteria were atypical Parkinsonism, cognitive impairment (MMSE < 24/30), severe disability (H&Y stage >4), or other diseases causing acute or chronic pain. Spearman’s rank correlation coefficient and multiple regression were used for data analysis.
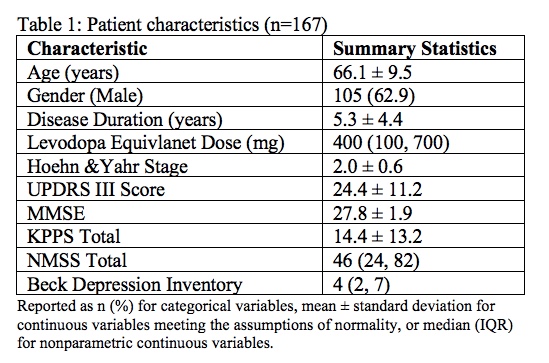
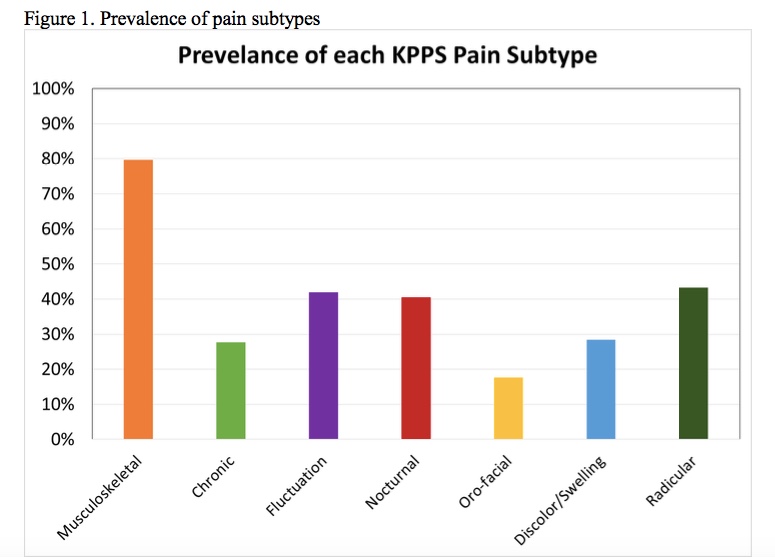
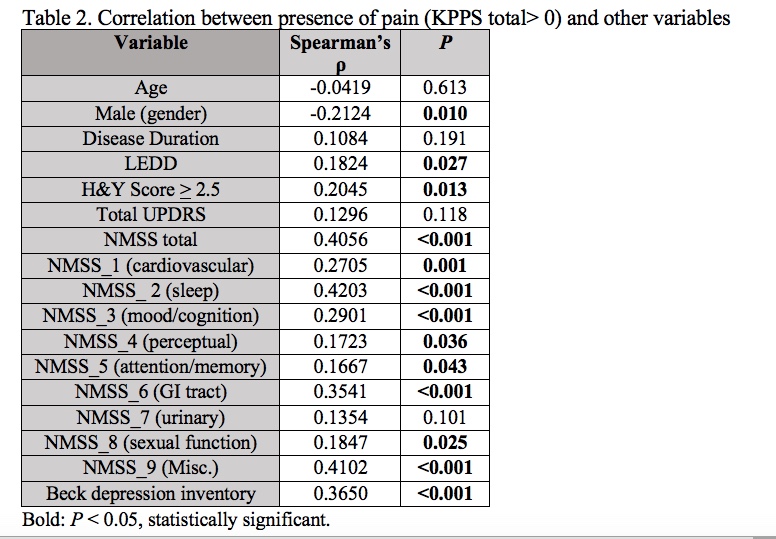
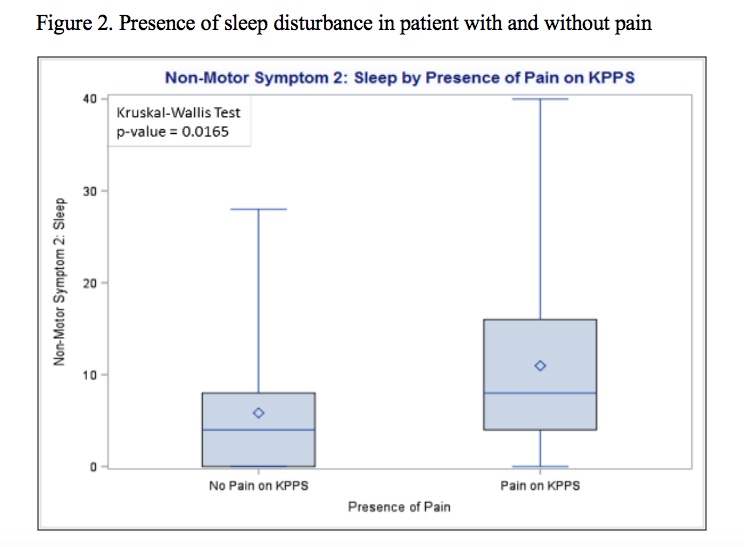
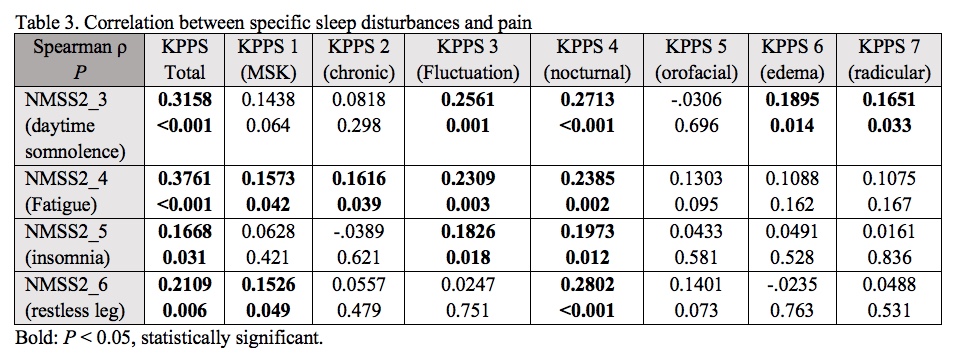
Results: 167 patients were enrolled (Table 1) and 88.6% (n=148) experienced pain (defined as KPPS total > 0) with musculoskeletal pain being most prevalent (Figure 1). Pain correlated with multiple NMS (Table 2), and had the strongest correlation with sleep disruption (NMSS-2). Multiple regression analysis (F=19.95; P<0.001) with R2=0.42 revealed independent associations between pain and female gender (P=0.003), cardiovascular disturbance (P=0.001), and sleep disruption (P<0.001). The independent association between pain and sleep persisted in the subgroup of pain patients on dopaminergics (n=126; P=0.001). Patients with pain had significantly higher sleep disruption scores than those without pain (median 8 vs. 4; P=0.017; Figure 2). Further analysis of specific sleep disturbances showed that fatigue had the strongest correlation with pain and correlated across multiple pain subtypes (Table 3).
Conclusion: Pain is highly prevalent in PD and is independently associated with sleep disruption, even in those treated with dopaminergics. This suggests that pain may be linked to sleep disruption, particularly fatigue. While pain may lead to poor sleep quality, it is also possible that pain and sleep disruption share a common pathophysiology[4] or that sleep disruption may lower the pain threshold. Moreover, treating pain in PD may also require addressing related NMS.
References: 1 Ford, B. (2010). Mov Disord 25 Suppl 1: S98-103. 2 Silverdale, M. A., et al. (2018). Parkinsonism Relat Disord 56: 27-32. 3 Antonini, A., et al. (2018). Eur J Neurol 25(7): 917-e969. 4 Martinez-Martin, P., et al. (2019). Mov Disord Clin Pract 6(1): 57-64. 5 Sauerbier, A., et al. (2016). Parkinsonism Relat Disord 22 Suppl 1: S41-46.
To cite this abstract in AMA style:
P. Ghosh, P. Imbriani, N. Caputi, L. Covington, A. Sparks, T. Schirinzi, Y. Salnikova, S. Natoli, A. Pisani. A Dual-Center Study of Pain and Other Non-motor Symptoms in Parkinson disease [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/a-dual-center-study-of-pain-and-other-non-motor-symptoms-in-parkinson-disease/. Accessed December 28, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/a-dual-center-study-of-pain-and-other-non-motor-symptoms-in-parkinson-disease/