Category: Neuroimaging (Non-PD)
Objective: Highlight the clinical features and radiologic findings of diabetic striatopathy.
Background: Diabetic striatopathy is a rare condition associated with chorea and/or ballism but can have reversible abnormalities in neuroimaging. [1,2] Prevalence rates in the literature have been reported as 1 in 100,000 but given the low familiarity with this syndrome, this can be inaccurate. [2] Treatment of this condition typically involved glycemic control and medications for chorea.
Method: Describe a case of diabetic striatopathy, its clinical presentation, radiographic findings, and management strategies. Also, highlight some controversies regarding findings on CT and MRI.
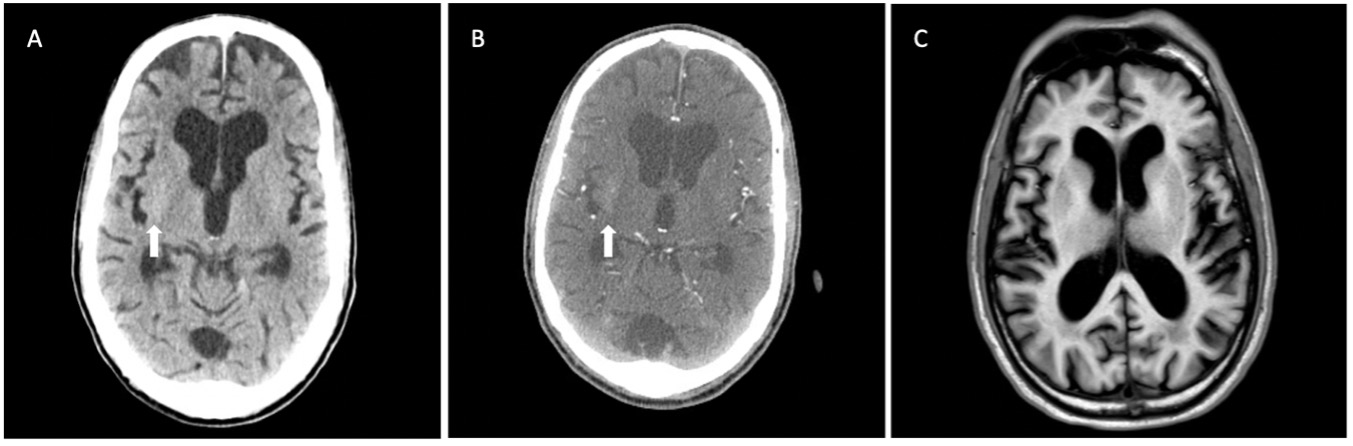
Results: A 69-year-old African American man with no known past medical history was brought to the ED after being found unresponsive. EMS was called and reported to have witnessed what seemed to be seizure-like activity on the left side of his body. On admission the patient’s BP was 110/56 mmHg and his HR 55 BPM, with a GCS score of 3. He was intubated for airway protection and his blood glucose was found to be 1021 mg/dL, hemoglobin A1c was 13.8%. CT head and CTA were obtained and showed subtle asymmetric hyper-attenuation of the right putamen [figure 1]. The patient was started on an insulin drip and his hyperglycemia started improving. An EEG was completed and was compatible with severe diffuse encephalopathy without epileptiform discharges or lateralizing signs. A brain MRI 3 days after the CT did not show any acute abnormalities and no T1 hyperintense right putaminal signal to correspond to CT findings [figure 1]. The patient significantly improved and was discharged home with insulin therapy.
Conclusion: Diabetic striatopathy is a commonly misdiagnosed condition that can present with chorea and/or ballism or seizures. In 17.5% of cases there is CT and MRI mismatch. Since both modalities might show differential regional changes, CT is still indicated despite the absence of MRI findings. [2] Awareness of this condition can increase prompt treatment and better outcomes for the patients, as well as optimize resources in the clinical setting.
References: 1. Ryan, C., Ahlskog, J. E. & Savica, R. Hyperglycemic chorea/ballism ascertained over 15 years at a referral medical center. Park. Relat. Disord. 48, 97–100 (2018).
2. Chua, C. B. et al. “Diabetic striatopathy”: clinical presentations, controversy, pathogenesis, treatments, and outcomes. Sci. Rep. 10, 1–11 (2020).
To cite this abstract in AMA style:
J. Patino, A. Durand, R. Samudralwar. A 69-year-old man with seizure-like activity and unresponsiveness [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/a-69-year-old-man-with-seizure-like-activity-and-unresponsiveness/. Accessed February 3, 2026.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/a-69-year-old-man-with-seizure-like-activity-and-unresponsiveness/