Session Information
Date: Tuesday, June 21, 2016
Session Title: Rare genetic and metabolic diseases
Session Time: 12:30pm-2:00pm
Location: Exhibit Hall located in Hall B, Level 2
Objective: To evaluate clinical, biochemical and imaging profile of patients with Wilson’s Disease (WD).
Background: There was no reported case series of WD in Myanmar.This study was a hospital –based study carried out at Department of Neurology, Yangon General Hospital, Myanmar.
Methods: During the period of 2010 to 2015,17patients were diagnosed with definitive WD and one had likely WD by using Leipzig criteria.
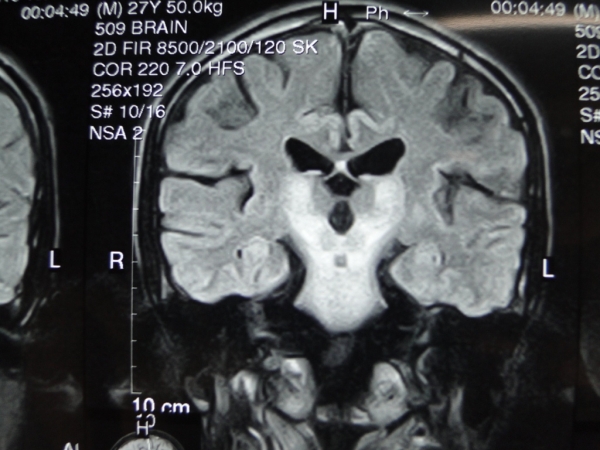
Results: Of the18 patients 8 were males and 10 were females.Mean age at the time of diagnosis was 20 years.Main presenting features were:abnormal gait in 17 out of 18 (94.4%);speech problems17(94.4%),Parkinsonian features 9(50%),tremor 8(44.4%),cerebellar symptoms and signs in 4(22.2%).Fourteen patients(66.6%) had psychiatric symptoms.Five patients(27.7%) had swallowing difficulty,2(11.1%) had seizures and1(5.5%)had chorea.KF rings were positive in all patients.Serum ceruloplasmin level was low in17(94.4%) patients and lower normal limit in one patient.Only 3 patients(16.6 %) had coexisting hepatic manifestation.Renal and haematological involvement was seen in 2 patients(11.1%).Three(16.6%) patients had positive family history and one patient (5.5%) had consanguineous marriage of the parents.Only one of the siblings of affected patients was screened and found to have WD.CT (Brain) was done in 8 out of 18 patients(44.4%) and all had bilateral basal ganglia hypodensity and one(5.5%) had subcortical involvement.MRI (Brain) was done in 12 out of 18 patients(61.1%) and showed hyperintense signals inT2 mainly in basal ganglia, thalami and mid brain. All patients were treated with penicillamine initially and zinc as a maintenance therapy.One patient had 12- week pregnancy at the time of diagnosis and penicillamine was given as trientine is not available.Her neurological symptoms markedly improved and but she had premature delivery at 34 weeks.The child was low-birth weight with hypotonia and passed away at one year old.Only 7out of 18 patients (38.8%) came for regular follow- up and clinical improvements were seen but the outcome of eleven patients were not known.
Conclusions: The limited access to diagnostic facilities and availability of drugs is a major barrier for the early diagnosis and compliance of long term treatment leading to devastating consequences of the disease in patients in this study. References: 1. Ferenci P. et al: EASL Clinical Practice Guidelines: Wilson’s disease. Journal of Hepatology 2012 vol.671-685.
To cite this abstract in AMA style:
S.M.M. Aye, K.M.P.P. Kyaw, Z. Myint Shwe, O. Ohnmar, Y.M. Aye, W.M. Thit. Clinical profile of Wilson’s disease at Yangon General Hospital, Myanmar [abstract]. Mov Disord. 2016; 31 (suppl 2). https://www.mdsabstracts.org/abstract/clinical-profile-of-wilsons-disease-at-yangon-general-hospital-myanmar/. Accessed April 2, 2025.« Back to 2016 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-profile-of-wilsons-disease-at-yangon-general-hospital-myanmar/
