Session Information
Date: Monday, June 20, 2016
Session Title: Epidemiology
Session Time: 12:30pm-2:00pm
Location: Exhibit Hall located in Hall B, Level 2
Objective: To develop and validate a prognostic model to predict mortality in Parkinson’s disease (PD).
Background: Most previous prognostic studies in PD have used unrepresentative cohorts with selection biases resulting in heterogeneous mortality estimates and limited identification of prognostic factors. Prognosis is best studied by long-term follow-up of community-based incident cohorts. Prognostic models can be used to predict patients’ risk, correct for case mix, and improve clinical trial design (eg, selection of patients or stratification of randomisation by prognosis), but no prognostic model (for any outcome) has been published for use in PD.
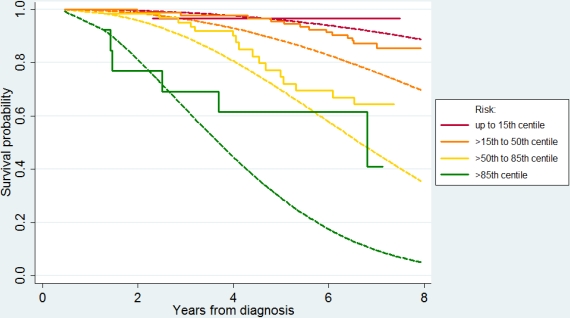
Methods: The PINE study and the ParkWest study are both community-based, incidence cohorts of PD with lifelong prospective follow-up in North-East Scotland and Western Norway, respectively. In each study area, all incident cases were identified with multiple, community-based ascertainment strategies (during 2004-6 & 2006-9 in PINE and 2004-7 in ParkWest). Weibull regression was used to create a prognostic model for mortality using data from the PINE cohort with clinical predictors measured at time of diagnosis. It was externally validated by measuring calibration (observed versus predicted survival in quantiles of predicted risk) and discrimination (C-statistic) in the ParkWest cohort.
Results: In the PINE study, 91 of 198 incident PD cases died after follow-up between 6 and 12 years. Independent baseline prognostic factors were age, male sex, higher co-morbidity (with effect in the earlier part, but not later part, of follow-up), more bradykinesia, and more axial relative to limb features (see table
| Baseline variable | Hazard ratio (95% confidence interval) | P-value |
| Age at diagnosis (10-year increase) | 1.91 (1.43–2.54) | <0.001 |
| Sex (male vs female) | 1.84 (1.17–2.91) | 0.009 |
| Bradykinesia score (5-point increase) | 1.40 (1.14–1.72) | 0.002 |
| Axial:limb ratio (1-unit increase) | 1.81 (1.22–2.68) | 0.003 |
| Charlson score (effect up to 4 years) | 1.33 (1.14–1.56) | <0.001 |
| Charlson score (effect after 4 years) | 0.83 (0.63–1.09) | 0.17 |
| Shape parameter | 2.36 (1.96–2.83) | <0.001 |
| Constant | -5.86 (-6.8–-4.89) | <0.001 |
 ).
).
Conclusions: Overall mortality risk was higher in the PINE study. The prognostic model had good discrimination and can therefore be used for case-mix correction or patient selection/stratification according to prognosis in trials. Because the model tended to underestimate survival in the validation cohort, recalibration of the model may be necessary before it is used for individualised risk prediction in other settings.
To cite this abstract in AMA style:
A.D. Macleod, I. Dalen, O.B. Tysnes, J.P. Larsen, C.E. Counsell. Development and external validation of a prognostic model of mortality in Parkinson’s disease [abstract]. Mov Disord. 2016; 31 (suppl 2). https://www.mdsabstracts.org/abstract/development-and-external-validation-of-a-prognostic-model-of-mortality-in-parkinsons-disease/. Accessed December 13, 2025.« Back to 2016 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/development-and-external-validation-of-a-prognostic-model-of-mortality-in-parkinsons-disease/
