Objective: To determine the prevalence of apraxia of eyelid opening (AOELO) in patients with movement disorders evaluated at the Parkinson’s Disease Center and Movement Disorders Clinic, Baylor College of Medicine, Houston, TX, and to explore its demographic and clinical correlates.
Background: AOELO is the inability to voluntarily open the eyes in the absence of orbicularis oculi (OO) contraction, despite sustained frontalis contraction. Electrophysiologic studies have suggested it is due to an excessive inhibition of the levator palpebrae superioris muscle without evidence of ongoing OO activity. However, the exact pathophysiology remains unclear and several other terms including involuntary levator palpebrae inhibition, blepharocolysis, akinesia and freezing of eyelids, and atypical blepharospasm have been used to describe it. It is still not clear whether the underlying pathophysiology of AOELO is apraxia, dystonia, or both, therefore the topic deserves to be revisited.
Method: We searched our meticulously organized video library of patients recorded from 2006 to present and searched for patients with AOELO. We also collected data about primary diagnoses, co-existing movement and other neurological disorders, demographics, and botulinum toxin (BoNT) injections.
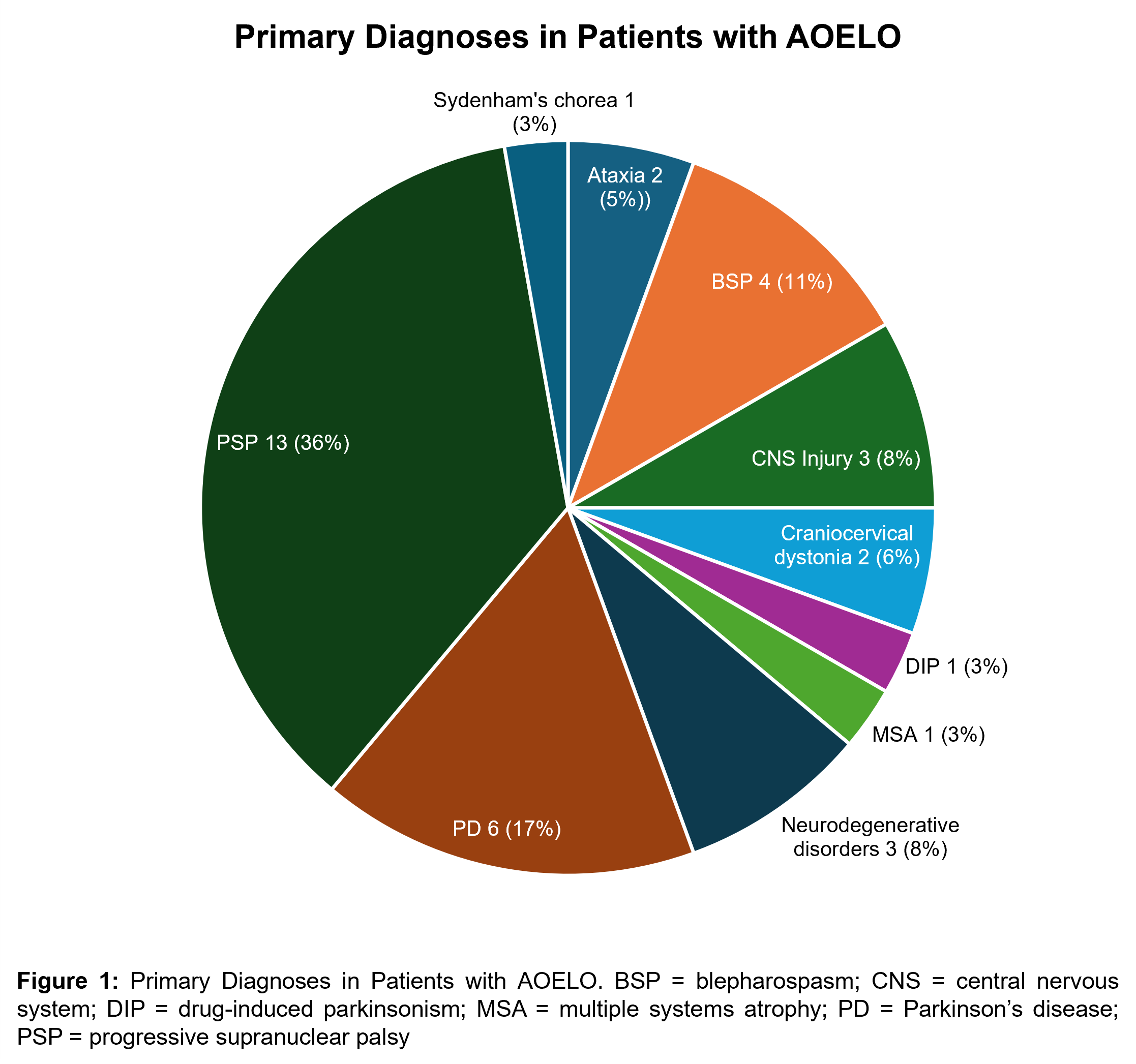
Results: We found 36 patients (55.6% male; mean age: 61.2 ± 17.9) with AOELO. The most common primary diagnoses were progressive supranuclear palsy (PSP) (36%), idiopathic Parkinson’s disease (PD) (17%), followed by BSP, CNS injuries due to hypoxic or vascular ischemia, and other neurodegenerative disorders, such as dementia with Lewy bodies, fronto-temporal dementia, spinal-cerebellar ataxia type 3, craniocervical dystonia, ataxia, Sydenham’s chorea, multiple system atrophy, and drug-induced parkinsonism [figure1]. Nearly half of our patients with AOELO (47.2%) had co-existent BSP. In 11 patients with follow up records, 2 received BoNT for AOELO and 9 for AOELO+BSP; 9 had excellent or partial improvement and 2 failed to respond.
Conclusion: In our cohort of 36 patients with AOELO, the most commonly associated movement disorders were PSP, followed by PD. Approximately, half of the patients had co-existent BSP. Further studies are needed to obtain deeper insights into the pathophysiology and treatment of AOELO.
Figure 1: Primary Diagnoses in Patients with AOELO
References: [1] Aramideh, M., Ongerboer de Visser, B. W., Devriese, P. P., Bour, L. J., & Speelman, J. D. (1994). Electromyographic features of levator palpebrae superioris and orbicularis oculi muscles in blepharospasm. Brain: A Journal of Neurology, 117 ( Pt 1), 27–38. https://doi.org/10.1093/brain/117.1.27
[2] Waln O, Jankovic J. Neuro-ophthalmology of movement disorders. Expert Review of Ophthalmology 2018;13(5):283–292.
[3] Hamedani, A. G., & Gold, D. R. (2017). Eyelid Dysfunction in Neurodegenerative, Neurogenetic, and Neurometabolic Disease. Frontiers in Neurology, 8, 329. https://doi.org/10.3389/fneur.2017.00329
[4] Tozlovanu, V., Forget, R., Iancu, A., & Boghen, D. (2001). Prolonged orbicularis oculi activity: A major factor in apraxia of lid opening. Neurology, 57(6), 1013–1018. https://doi.org/10.1212/wnl.57.6.1013
[5] Yoon, W. T., Chung, E. J., Lee, S. H., Kim, B. J., & Lee, W. Y. (2005). Clinical analysis of blepharospasm and apraxia of eyelid opening in patients with parkinsonism. Journal of Clinical Neurology (Seoul, Korea), 1(2), 159–165. https://doi.org/10.3988/jcn.2005.1.2.159
[6] Zarifkar P, Shaff NA, Nersesjan V, Mayer AR, Ryman S, Kondziella D. Lesion network mapping of eye-opening apraxia. Brain Commun. 2023 Oct 27;5(6):fcad288.
To cite this abstract in AMA style:
H. Conn, A. Lenka, J. Jankovic. Apraxia of eyelid opening in patients with movement disorders [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/apraxia-of-eyelid-opening-in-patients-with-movement-disorders/. Accessed February 28, 2026.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/apraxia-of-eyelid-opening-in-patients-with-movement-disorders/