Category: Parkinson's Disease: Neuroimaging
Objective: To apply an AI model in a multi-site longitudinal study to segment substantia nigra pars compacta (SNpc), perform longitudinal analysis, and quantify its association with clinical scores.
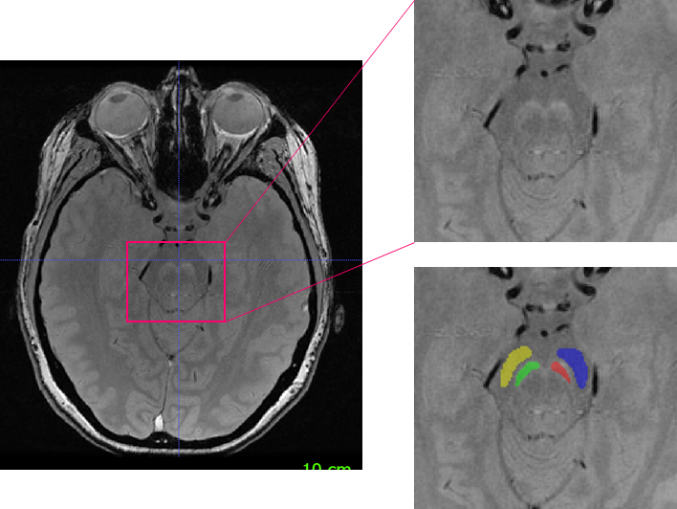
Background: The degeneration of dopaminergic neurons in the SNpc manifests as depigmentation of the SNpc and can be captured via neuromelanin MRI (NM-MRI) [1,2,3]. Here, we employ an in-house trained AI model to segment the SNpc and perform a post-hoc analyses on data acquired from a large multi-center clinical trial in PD patients (SPARK; NCT03318523) [4].
Method: 170 of 330 subjects from the SPARK study with PD diagnosis ≤3 yrs, a modified H&Y score ≤2.5, had no symptomatic treatment within 12 weeks, and abnormal striatal DaTscan uptake, and with 3 assessable and sufficient quality timepoints (screening, week-24, week-52) were included. NM-MRI was acquired at 80 sites with 3T capabilities using a 3D-GRE sequence (Fig. 1). Using a trained and validated AI model [5], SNpc and a cerebral peduncle reference region (RR) were auto segmented, and volume and contrast ratio (CR) were computed. The mean intensity (I) of the SNpc and RR was used to compute the CRs ((ISNpc-IRR)/IRR). An ANOVA model was employed to test for significant volume and CR change. Linear partial regression was used to understand the relation between imaging markers and MDS-UPDRS total score controlling for age. Lasso regularization with 5-fold cross-validation was used to optimize coefficients to combine all imaging measures of interest into a single variable while minimizing variance in MDS-UPDRS.
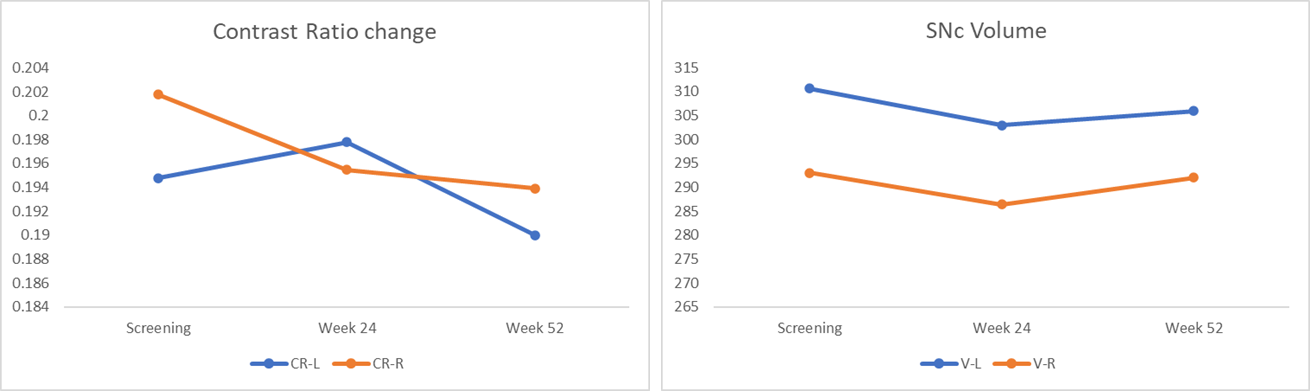
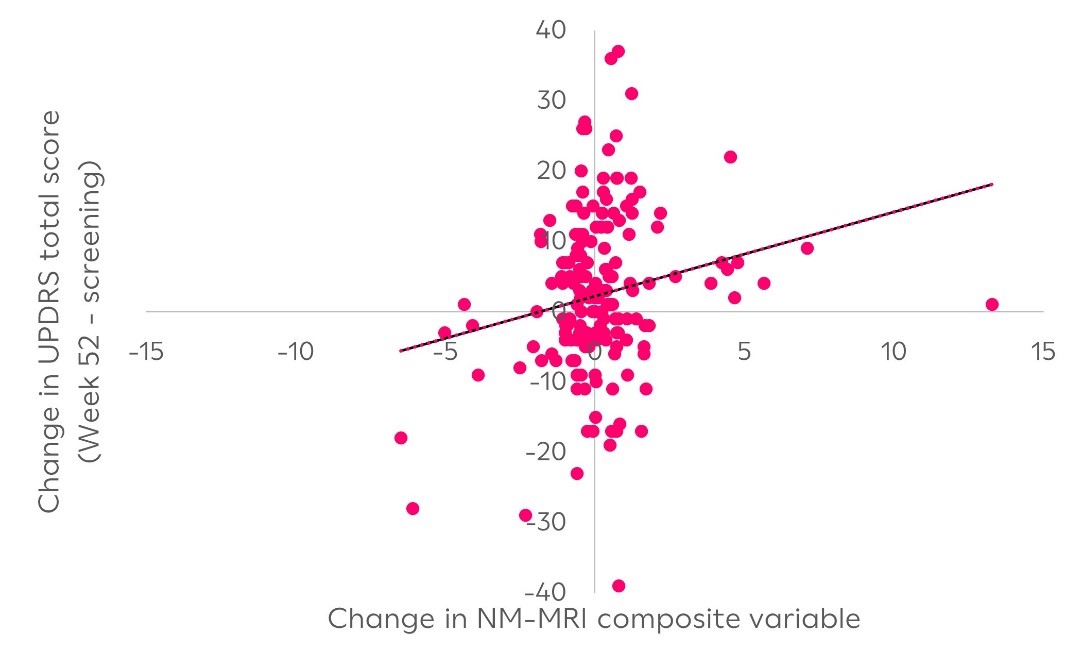
Results: The mean CR and the volume of SNpc decreased consistently over time [-2.51% ± 1.5]. A statistically significant difference from baseline in the right SNpc CR (p<0.05) at week-52. Age-corrected regression with MDS-UPDRS showed a significant negative correlation between within-subject change from baseline in the right CR at week-52 (r=-0.14, p<0.05). The lasso-composite variable demonstrated a highly significant association (p<0.005) between the change in imaging features and the change in UPDRS at week-52.
Conclusion: Clinical progression is more strongly linked with change in contrast ratio than volume, however the strongest association is observed via a weighted combination of both imaging features, making CR and volume both crucial to be measured in longitudinal setting.
AI based SNpc and background segmentation
Average CR,Volume change from baseline to week52
NM-MRI composite vs UPDRS change at week 52.
References: 1. Bloem, B. R., Okun, M. S., & Klein, C. (2021). Parkinson’s disease. The Lancet, 397(10291), 2284-2303.
2. Damier, P., Hirsch, E. C., Agid, Y., & Graybiel, A. (1999). The substantia nigra of the human brain: II. Patterns of loss of dopamine-containing neurons in Parkinson’s disease. Brain, 122(8), 1437-1448.
3. Sasaki, M., Shibata, E., Tohyama, K., Takahashi, J., Otsuka, K., Tsuchiya, K., … & Sakai, A. (2006). Neuromelanin magnetic resonance imaging of locus ceruleus and substantia nigra in Parkinson’s disease. Neuroreport, 17(11), 1215-1218.
4. Hutchison RM, Fraser K, et al. (2024). Cinpanemab in Early Parkinson Disease: Evaluation of Biomarker Results From the Phase 2 SPARK Clinical Trial. Neurology. Mar 12;102(5):e209137.
5. Ingalhalikar M, Pham H, et al. “AI based neuromelanin MRI analysis in a multi-site longitudinal Parkinson’s Disease study” ISMRM 2024, Singapore.
To cite this abstract in AMA style:
M. Ingalhalikar, H. Pham, T. G, L. Bracoud, MH. Hutchison, K. Evans, T. Dam, KN. Nguyen, CC. Conklin, JS. Suhy, DS. Scott. AI based longitudinal changes in substantia nigra contrast and volume on neuromelanin MRI and its relation to clinical markers in a multi-site Parkinson’s disease study. [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/ai-based-longitudinal-changes-in-substantia-nigra-contrast-and-volume-on-neuromelanin-mri-and-its-relation-to-clinical-markers-in-a-multi-site-parkinsons-disease-study/. Accessed December 28, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/ai-based-longitudinal-changes-in-substantia-nigra-contrast-and-volume-on-neuromelanin-mri-and-its-relation-to-clinical-markers-in-a-multi-site-parkinsons-disease-study/