Category: Neuroimaging (Non-PD)
Objective: To describe the investigation and management of a patient with Wilson’s disease who experienced late-onset neurological deterioration despite continued treatment.
Background: Wilson’s disease is an autosomal–recessive disorder of copper metabolism, resulting in toxic accumulation of copper in various tissues. Neurological manifestations of copper excess can produce symptoms such tremor, parkinsonism and bulbar features. Management approaches include chelation with medication such as penicillamine, as well as antagonism of exogenous copper absorption with zinc salts. Paradoxical neurological deterioration can occur in up to 60% of patients after initiation of anti-copper therapy, and typically within 3 months of commencement. Late neurological worsening occurring more than 6 months after initiation of anti-copper treatment is rare.
Method: A 40-year-old lady with a known history of Wilson’s disease diagnosed at 18-years old presented with a 3-month history of bilateral hand tremor and progressive gait disturbance. She claimed compliance to her anti-copper medications of penicillamine 500mg OM and zinc 50mg TDS. Examination revealed symmetrical upper limb rigidity and bradykinesia as well as a postural wing-beating tremor on the right arm. There was no evidence of weakness or cerebellar signs.
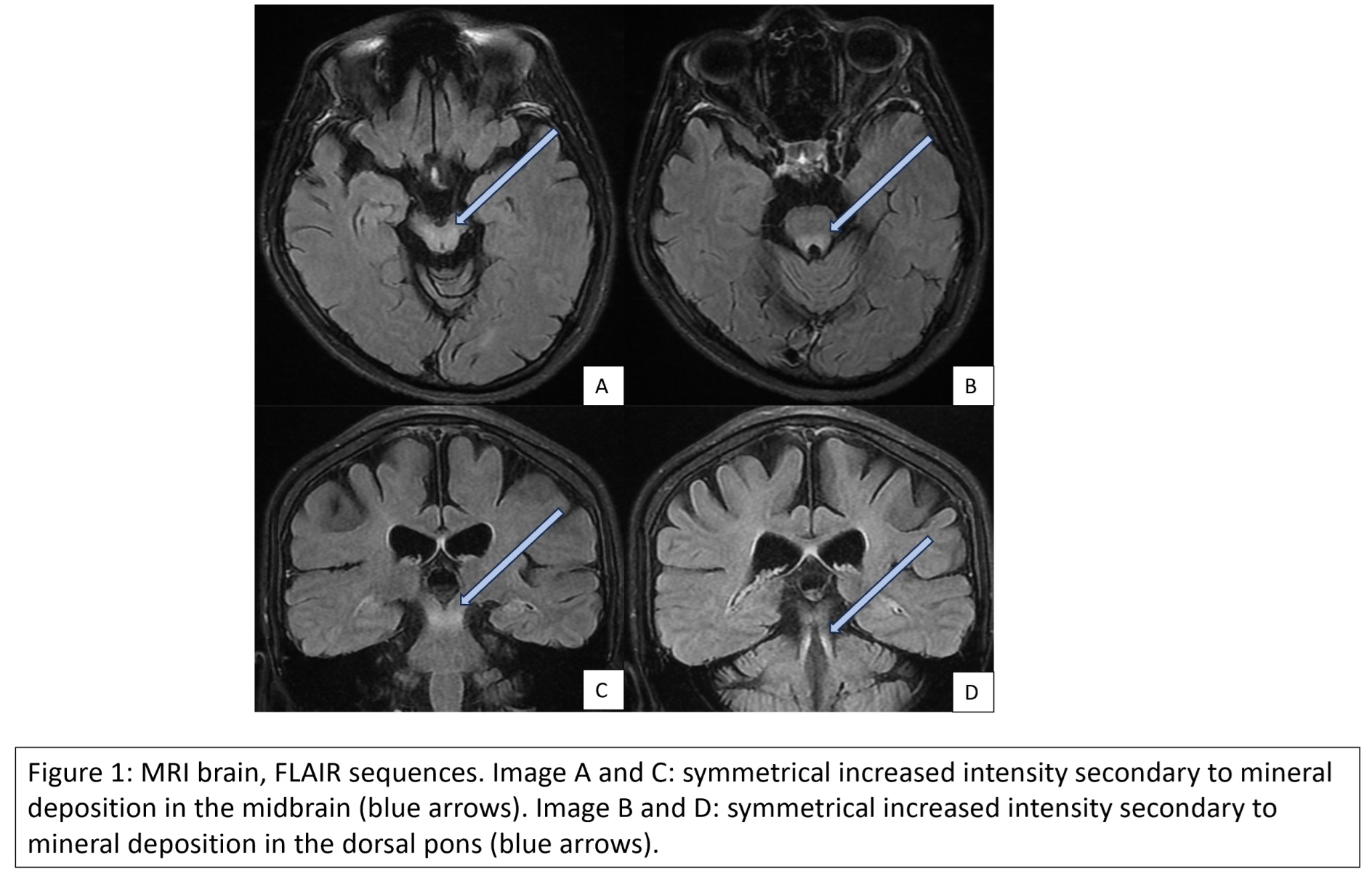
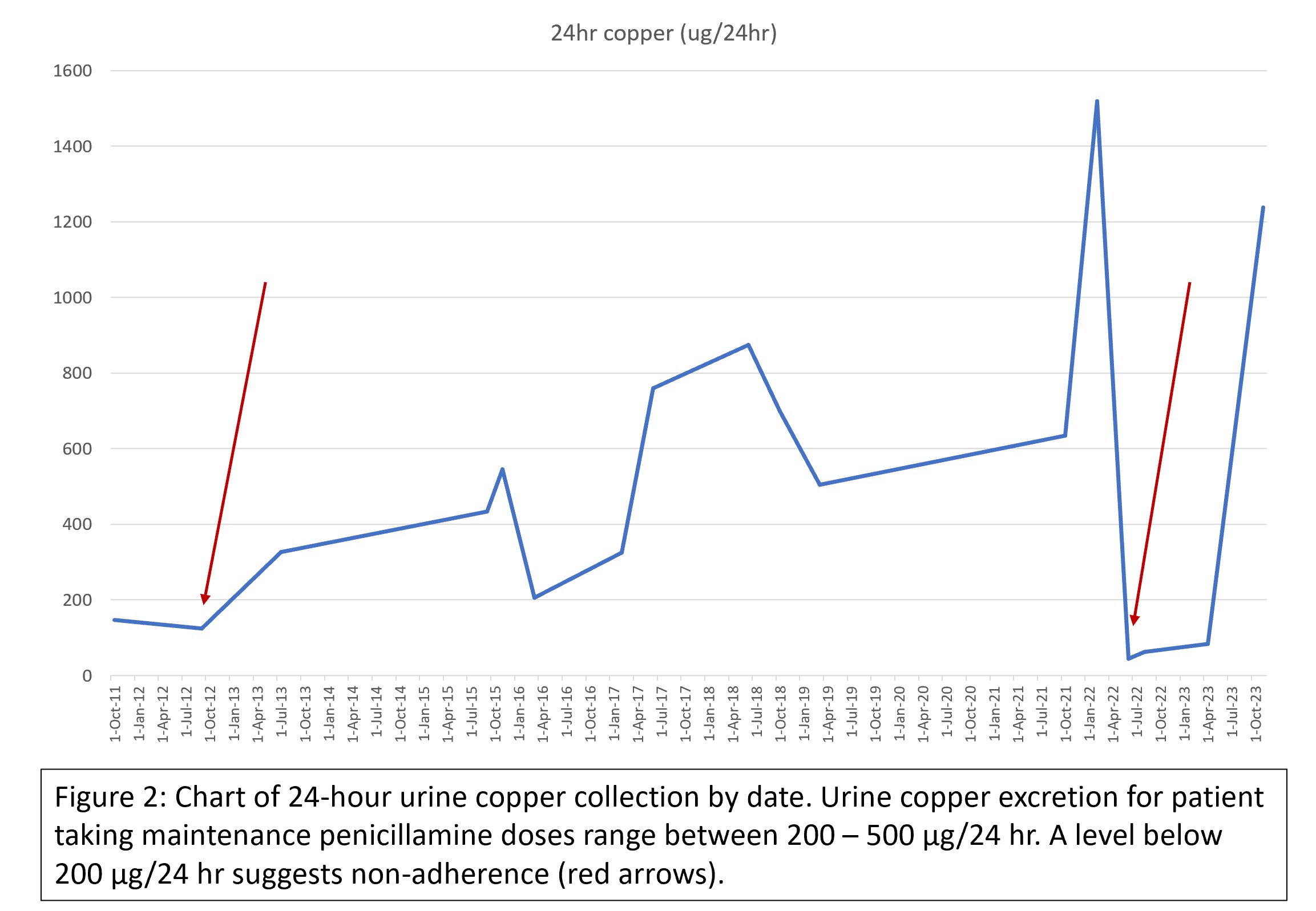
Results: Brain MRI revealed bilateral symmetrical increased T2/FLAIR signal in bilateral cerebral peduncles, midbrain and dorsal pons (Figure 1). These characteristic changes were stable from prior MRIs. A 24-hour urine copper collection showed a urinary copper excretion of 83.9 µg/24hr. This result was unusually low, considering that patient was on long-term treatment with both zinc salts as well as penicillamine. A review of our patient’s medical records revealed previous episodes of non-compliance, with reemergence of neurological symptoms and low 24-hour urine copper collections (Table 1). Medication adherence was strongly emphasised. On repeat visit, her neurological symptoms remained stable, and 24-hour urine copper collection had surged to 19.48 µmol/24hr (1,237 µg/24hr). We diagnosed neurological deterioration secondary to poor adherence to anti-copper medications.
Conclusion: The most common cause of late neurological deterioration in Wilson’s disease is non-adherence to treatment. Regular laboratory monitoring and continued vigilance for recurrence of neurological symptoms of copper excess is essential for early detection and treatment.
Figure 1: MRI brain, FLAIR sequences
Figure 2: Chart of 24-hour urine copper collection
To cite this abstract in AMA style:
D. Tang, CH. Tan, SF. Woo, D. Soon, J. Tan. A Curious Case of Copper de-Compensation [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/a-curious-case-of-copper-de-compensation/. Accessed December 26, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/a-curious-case-of-copper-de-compensation/