Category: Epidemiology
Objective: To determine the validity of PD diagnostic codes in a large national electronic medical database and develop recommendations for maximizing ascertainment accuracy.
Background: EMR-based case-finding typically ascertains PD using ICD codes. Few studies consider the potential impact of diagnostic misclassification despite well documented limitations.[1]
Method: As part of an ongoing study, we investigated a cohort of 146,776 veterans who utilized VA healthcare between 1999-2021.[2] We identified individuals with any ICD9 (332.0) or ICD10 (G20) diagnostic code for PD in outpatient, inpatient, or community care settings. For each code we extracted encounter date, clinic and provider type. We also identified all patients who received prescriptions for dopaminergic medications. The medical records of each patient were reviewed to assign a gold-standard diagnosis using established criteria. We determined the positive predictive value (PPV) and sensitivity for several diagnostic combinations, and explored differences by race.
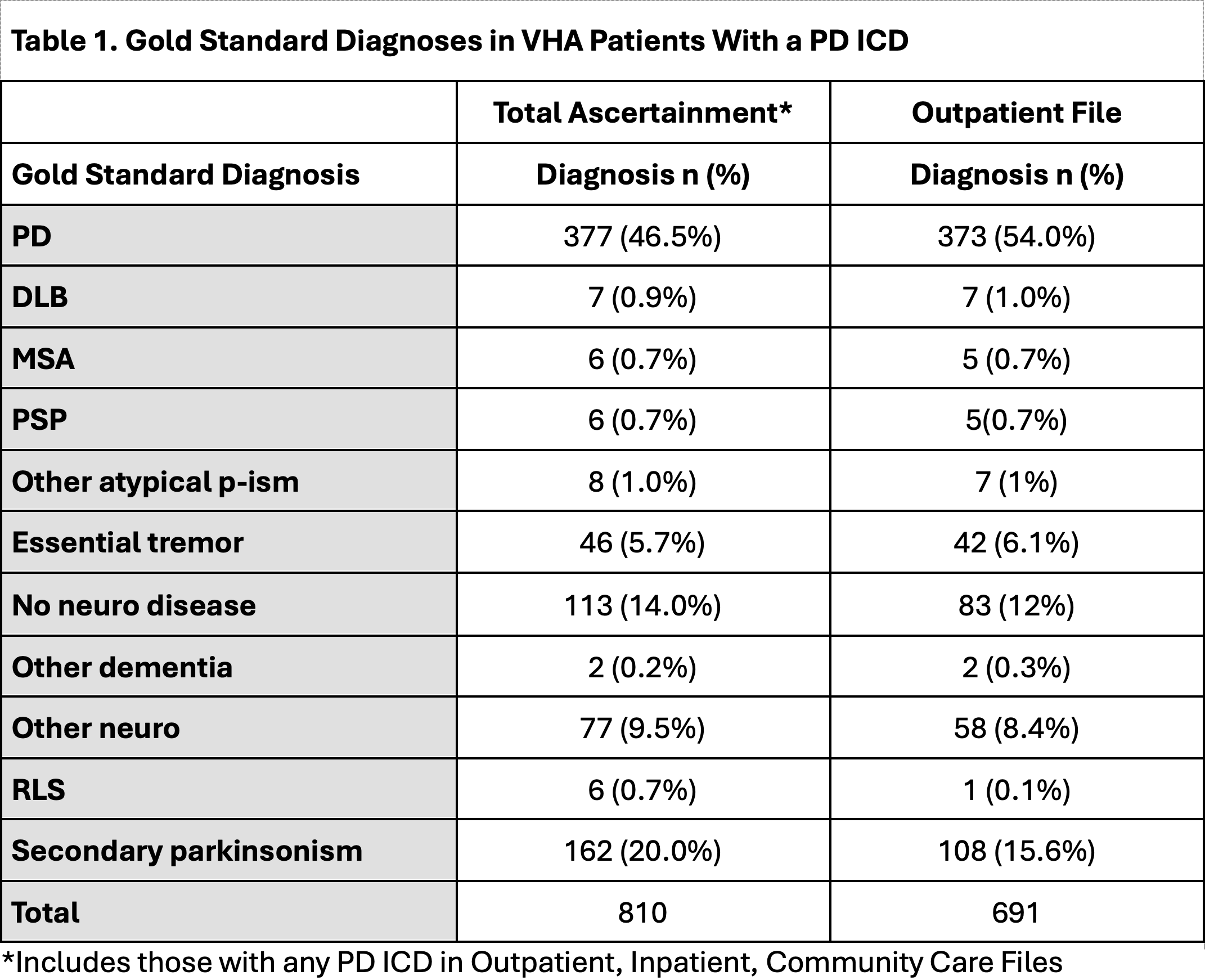
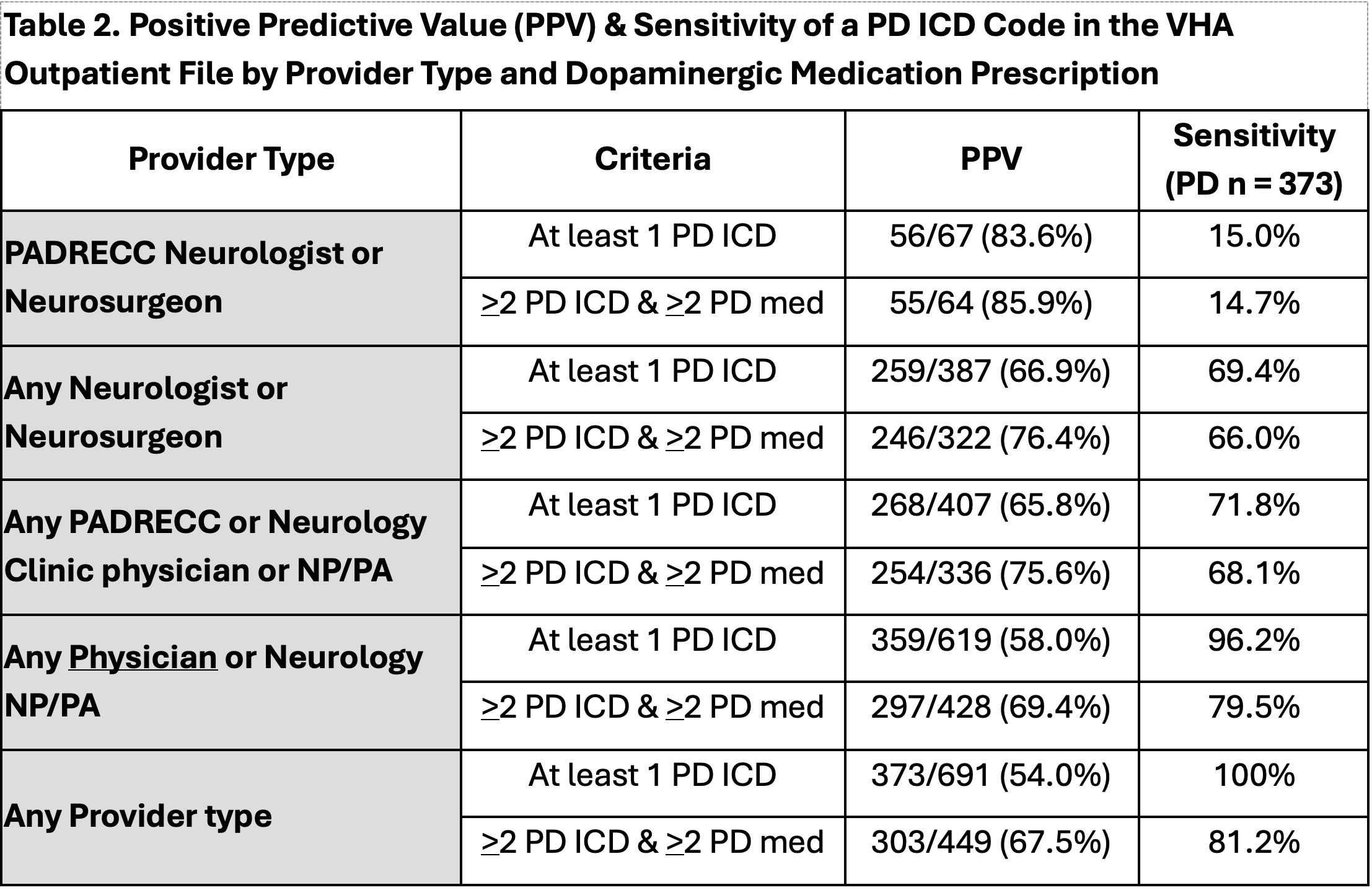
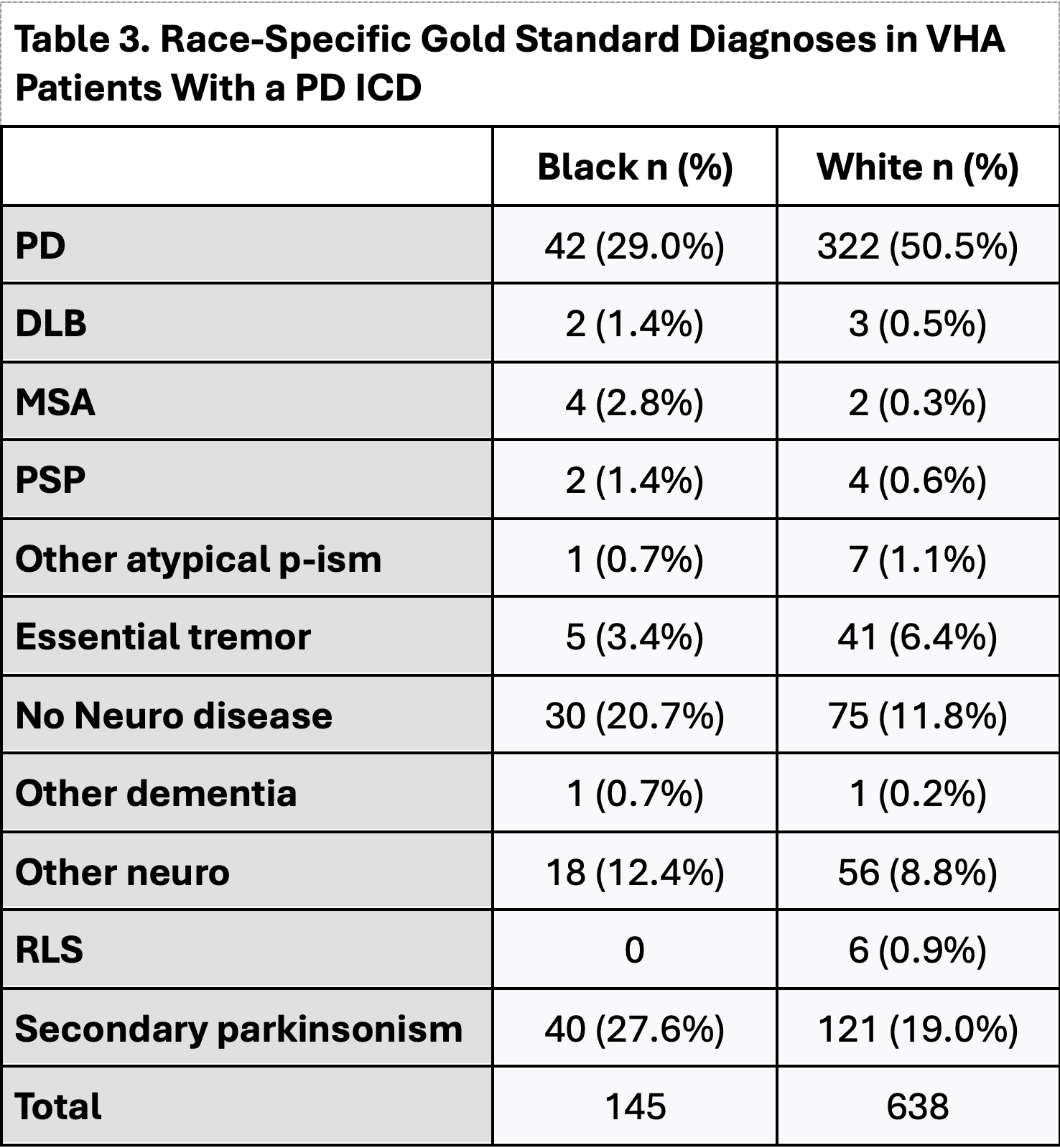
Results: 377 of 810 (PPV 46.5%) with a PD ICD code in any data source had PD, including 373 unique patients from outpatient files, 1 from inpatient, and 3 from community care.[table1] 18 additional cases were identified from pharmacy data alone. In analyses limited to outpatient data (n=691), veterans whose PD ICD was coded by a PADRECC-affiliated neurologist were most likely to have PD (PPV 83.6%), but sensitivity was poor (15.0%).[table2] Diagnostic accuracy decreased when considering PD coded by any neurologist (PPV 66.9%), but sensitivity was higher (69.4%). Requiring >=2 PD codes in combination with >= 2 levodopa prescriptions improved PPV modestly, particularly among non-neurologists, but also reduced sensitivity. Neuroleptic-induced parkinsonism was the most frequent diagnosis among those without PD (15.6%). Accuracy of a PD code was lower in Black (PPV 29.0%) than in White (PPV 50.5%) veterans regardless of provider type (miscoding OR 2.5, 95%CI 1.7-3.6).[table3]
Conclusion: These results highlight the limitations of EMR-based PD ascertainment. Better accuracy was established by requiring at least two ICD codes with medications, or coding by a PD-expert neurologist, at the cost of reduced sensitivity. Accuracy of non-neurologist-assigned PD codes is poor. Further investigation is warranted to understand the higher rate of miscoding among Black veterans.
Table 1.
Table 2.
Table 3.
References: [1] Harding Z, Wilkinson T, Stevenson A, Horrocks S, Ly A, Schnier C, Breen DP, Rannikmae K, Sudlow CLM. Identifying Parkinson’s disease and parkinsonism cases using routinely collected healthcare data: A systematic review. PLoS One. 2019;14(1).
[2] Goldman SM, Weaver FM, Stroupe KT, Cao L, Gonzalez B, Colletta K, Brown EG, Tanner CM. Risk of Parkinson Disease Among Service Members at Marine Corps Base Camp Lejeune. JAMA Neurol. 2023;80(7).
To cite this abstract in AMA style:
S. Goldman, F. Weaver, L. Cao, S. Jugnundan, B. Gonzalez, K. Stroupe, K. Colletta, E. Brown, C. Tanner. Validation of PD Ascertainment in the VA Electronic Medical Record (EMR) [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/validation-of-pd-ascertainment-in-the-va-electronic-medical-record-emr/. Accessed December 24, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/validation-of-pd-ascertainment-in-the-va-electronic-medical-record-emr/