Category: Parkinsonism, Others
Objective: To describe a stepwise evaluation of a patient with a secondary parkinsonism that mimic idiopathic Parkinson´s Disease (PD).
Background: PD clinically established encompasses the progression of motor and non-motor features. Some secondary parkinsonism phenotype closely resembles PD, therefore require a follow up to define the etiology.
Method: We report a case of a patient with parkinsonism admitted in emergency department and her follow up.
Results: A 59-year-old female admitted to the emergency department due to lethargy and somnolence that progressed six months prior to the admission. Her previous history had three years of progressive asymmetric left side slowness, rigidity, and tremor. Moreover, she developed an unstable, magnetic gait with frequent falls, urinary incontinence and mild cognitive complaints. Additionally, she had dream-enactment behavior suggestive of REM sleep behavior disorder (RBD).
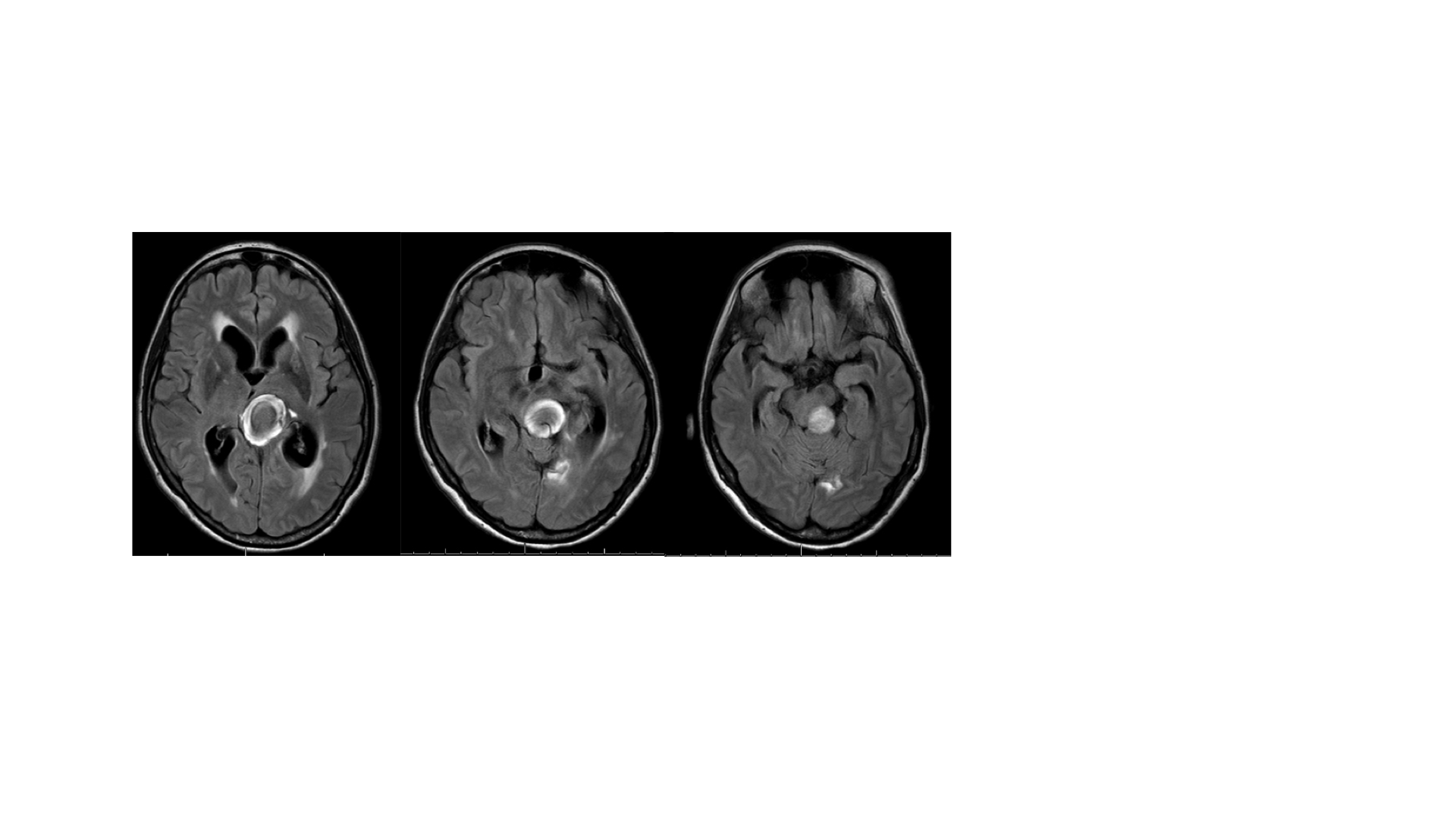
At the emergency she presented with drowsiness and left asymmetric parkinsonism. The investigation revealed a partial thrombosed posterior communicating artery aneurysm from the mesencephalon to the thalamus, causing hydrocephalus(Figure). A ventricular shunt was performed with improvement of cognitive deficits, magnetic gait, postural instability and urinary incontinence. At the follow-up, levodopa was titrated until 800 mg with no improvement of parkinsonism and maintenance of RBD.
Conclusion: At the initial assessment the parkinsonism was attributed to hydrocephalus and the mesencephalon mass. Nonetheless the persistence of symptoms subsequent to the resolution of hydrocephalus underscored the likelihood of an underlying associated PD, particularly given the high prevalence of RBD in synucleinopathies.
Conversely, during there was no improvement of parkinsonism with levodopa nor clinical progression, indicating that the persistent mass over the mesencephalon could be the cause parkinsonism and, consequently, an exclusionary criterion of PD.
Hence, although RBD is strongly associated with synucleinopathies, arising the concern of a underlaying synucleinopathy, our hypothesis this RBD may be attributed to the mechanical compression of locus coeruleus and dorsal raphe nucleus, neuroanatomical structures crucial in RBD networks.
In conclusion, we present a case exemplifying parkinsonism and RBD secondary a structural compression of regions implicated in synucleinopathies, potentially mimicking the clinical phenotype of PD.
Hydrocephalus secondary mass compression
Giant posterior communicating artery aneurysm
References: 1. Postuma, R. B. et al. MDS clinical diagnostic criteria for Parkinson’s disease: MDS-PD Clinical Diagnostic Criteria. Mov Disord. 30, 1591–1601 (2015).
2. Hughes, A. J., Daniel, S. E., Kilford, L. & Lees, A. J. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. Journal of Neurology, Neurosurgery & Psychiatry 55, 181–184 (1992).
3. Arnulf, I. REM sleep behavior disorder: Motor manifestations and pathophysiology. Mov. Disord. 27, 677–689 (2012).
4. Yuan, T., Zuo, Z. & Xu, J. Neuroanatomical Localization of Rapid Eye Movement Sleep Behavior Disorder in Human Brain Using Lesion Network Mapping. Korean J Radiol 24, 247 (2023).
To cite this abstract in AMA style:
A. Falcone, I. Brum, F. Freua, E. Barbosa, R. Cury, J. Parmera. Giant Aneurysm Causing Parkinsonism and REM Sleep Disorder [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/giant-aneurysm-causing-parkinsonism-and-rem-sleep-disorder/. Accessed March 29, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/giant-aneurysm-causing-parkinsonism-and-rem-sleep-disorder/