Category: Parkinsonism, Atypical: PSP, CBD
Objective: To test (1) the role of video oculography (VOG) in the detection of slow saccades in two common subtypes of Progressive Supranuclear Palsy (PSP) i.e. PSP-Parkinsonism (PSP-P) and PSP-Richardson syndrome (PSP-RS), and their differentiation from Parkinson’s disease (PD). (2) association between saccadic velocity or latency in VOG with scores of (a) PSP rating scale, (b) Montreal Cognitive Assessment (MoCA) and (c) Frontal assessment battery (FAB). (3) Estimate the frequency of apraxia of eye lid opening (ALO) and reflex blepharospasm in PSP and PD.
Background: PSP is clinically characterized by ocular motor dysfunction, postural instability, parkinsonism and cognitive impairment. Vertical gaze palsy or slowness of vertical more than horizontal saccades, is an important diagnostic feature of PSP and PSP subtypes according to MDS task force criteria.1 The role of VOG in any PSP subtype diagnosed using the new criteria has not been tested before.
Method: 112 PSP, 50 PD and 50 healthy controls participated in this single-centre, prospective, cross-sectional study. MDS-PSP1 and PD criteria2 were used respectively for the diagnosis. Only PSP-RS and PSP-P with slowness of saccades (level-O2) and not gaze palsy were included. Apraxia of eyelid opening (ALO) and the reflex blepharospasm were assessed clinically and using VOG.
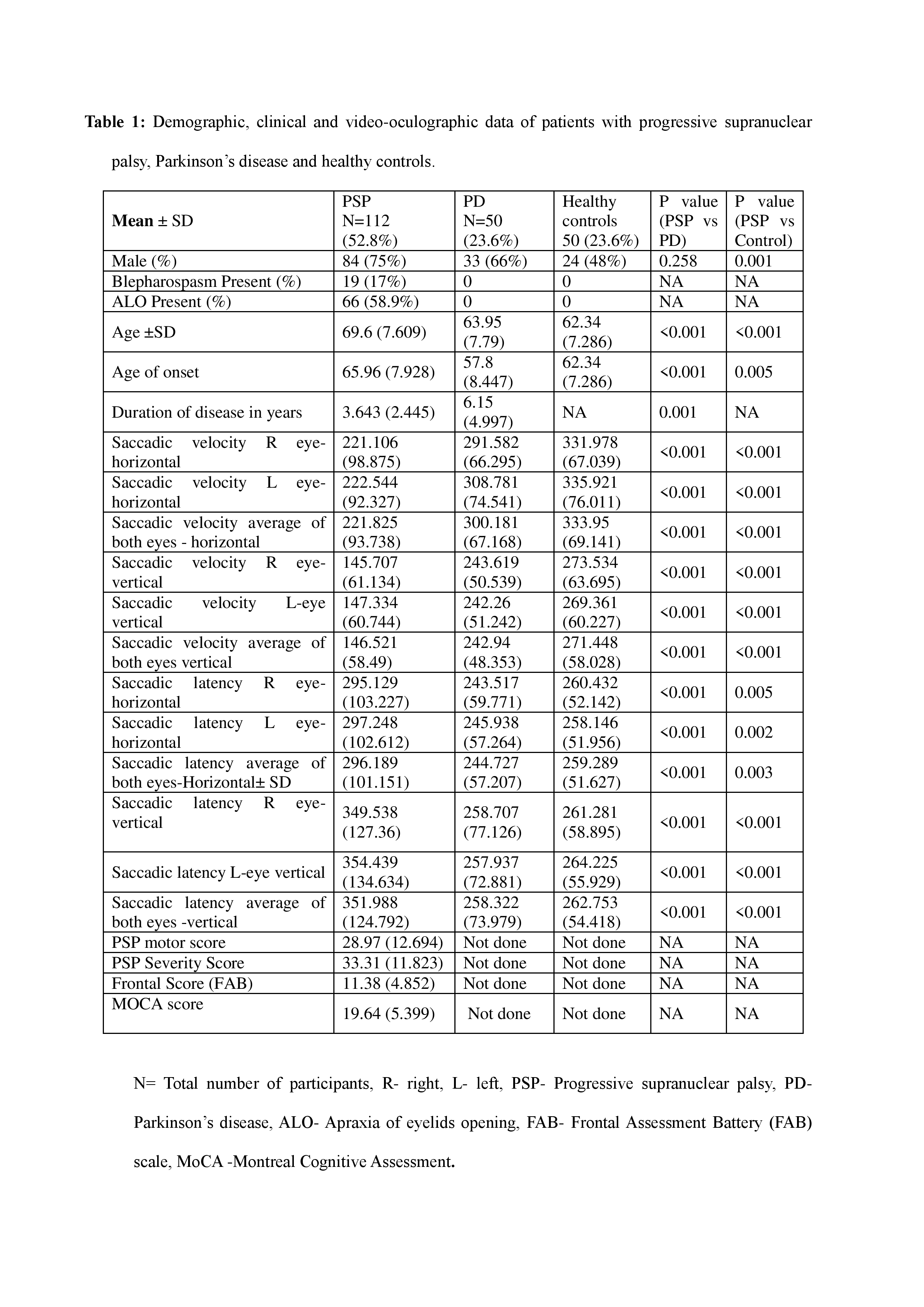
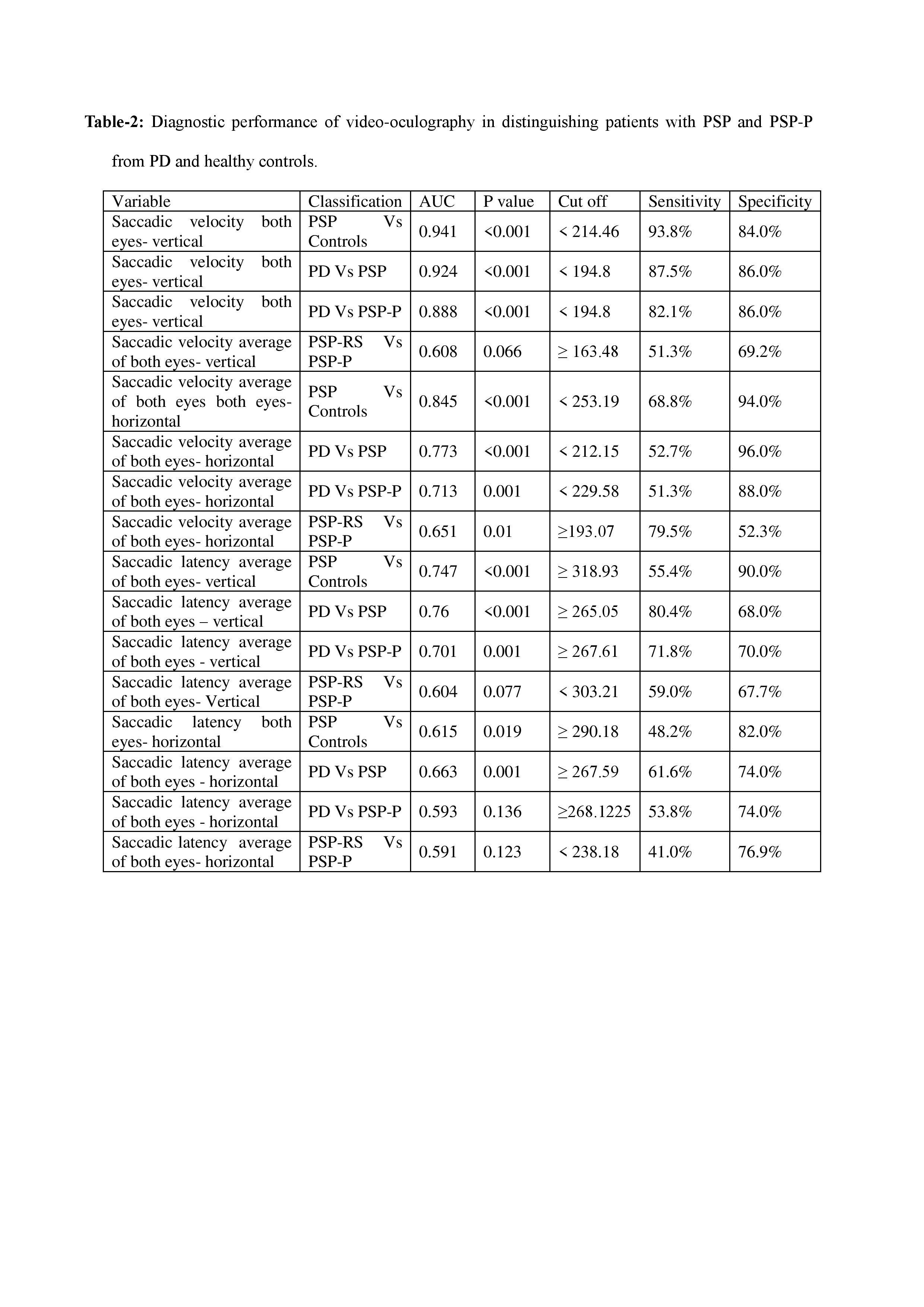
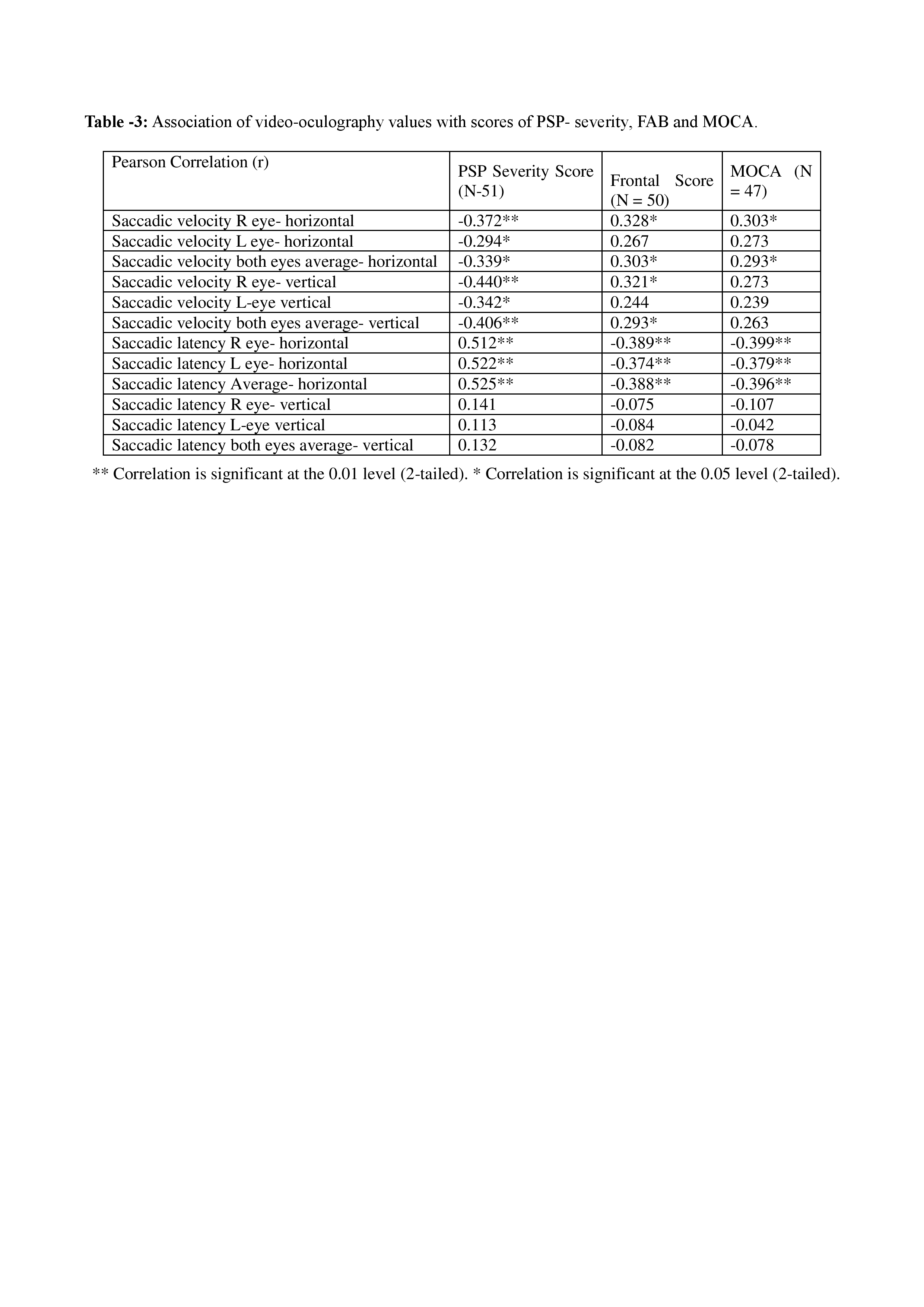
Results: Demographic, clinical and video-oculographic data of patients with PSP, PD and healthy controls are in table1. Horizontal and vertical saccadic velocities and latencies of each eye individually and together, differentiated PSP from both PD and healthy controls (P<0.001). Cutoff values of VOG, sensitivity, specificity and AUC in distinguishing PSP, PSP-P, PD and healthy controls from each other are shown in table 2. Vertical saccadic velocity and latency showed high accuracy in differencing PSP-P from PD. Worse scores of PSP severity, and cognition were seen in PSP-RS than in PSP-P. Worse PSP severity was associated with prolonged horizontal saccadic latency (table 3).
Conclusion: VOG is a useful tool for confirmation of clinically suspected or missed slow saccades in PSP- RS and PSP-P and in the differentiation of PSP-P from PD.
Table-1
Table-2
Table-3
References: 1. Höglinger GU, Respondek G, Stamelou M, Kurz C, Josephs KA, Lang AE, Mollenhauer B, Müller U, Nilsson C, Whitwell JL, Arzberger T. Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria. Movement Disorders. 2017 Jun;32(6):853-64.
2. Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G. MDS clinical diagnostic criteria for Parkinson’s disease. Movement disorders. 2015 Oct;30(12):1591-601.
To cite this abstract in AMA style:
H. Chovatiya, K. Pillai, C. Reddy, A. Prabhu, A. Thalakkattu, A. Avarachan, M. Chacko, A. Kishore. Video-oculography for enhancing the diagnostic accuracy of early oculomotor dysfunction in Progressive Supranuclear Palsy [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/video-oculography-for-enhancing-the-diagnostic-accuracy-of-early-oculomotor-dysfunction-in-progressive-supranuclear-palsy/. Accessed February 26, 2026.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/video-oculography-for-enhancing-the-diagnostic-accuracy-of-early-oculomotor-dysfunction-in-progressive-supranuclear-palsy/