Category: Parkinsonism, Atypical: PSP, CBD
Objective: We aim to assess diagnostic accuracy of the Parkinson-plus syndromes (PPS) using the current consensus criteria, whilst identifying the diagnostically most salient clinical features.
Background: Progressive supranuclear palsy (PSP), corticobasal syndrome (CBS) and multiple system atrophy (MSA) can be misdiagnosed in life, particularly in non-specialist clinics. Their clinical diagnostic criteria have been substantially revised within the last decade, though there have been very few prospective evaluations of diagnostic accuracy since.
Method: We studied 80 participants from the PROSPECT-M study, diagnosed with PPS in life and with a post-mortem examination. Post-mortem examination was undertaken at 1 of 4 UK Brain Banks. Demographics and both qualitative and quantitative clinical measures were compared, including MDS-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), PSP Rating Scale (PSPRS), Cambridge Behavioural Inventory (CBI) and the Montreal Cognitive Assessment (MoCA) scores. We compared clinical data across pathological groups and identified predictors of diagnosis using statistical multiple univariate logistic regression analysis.
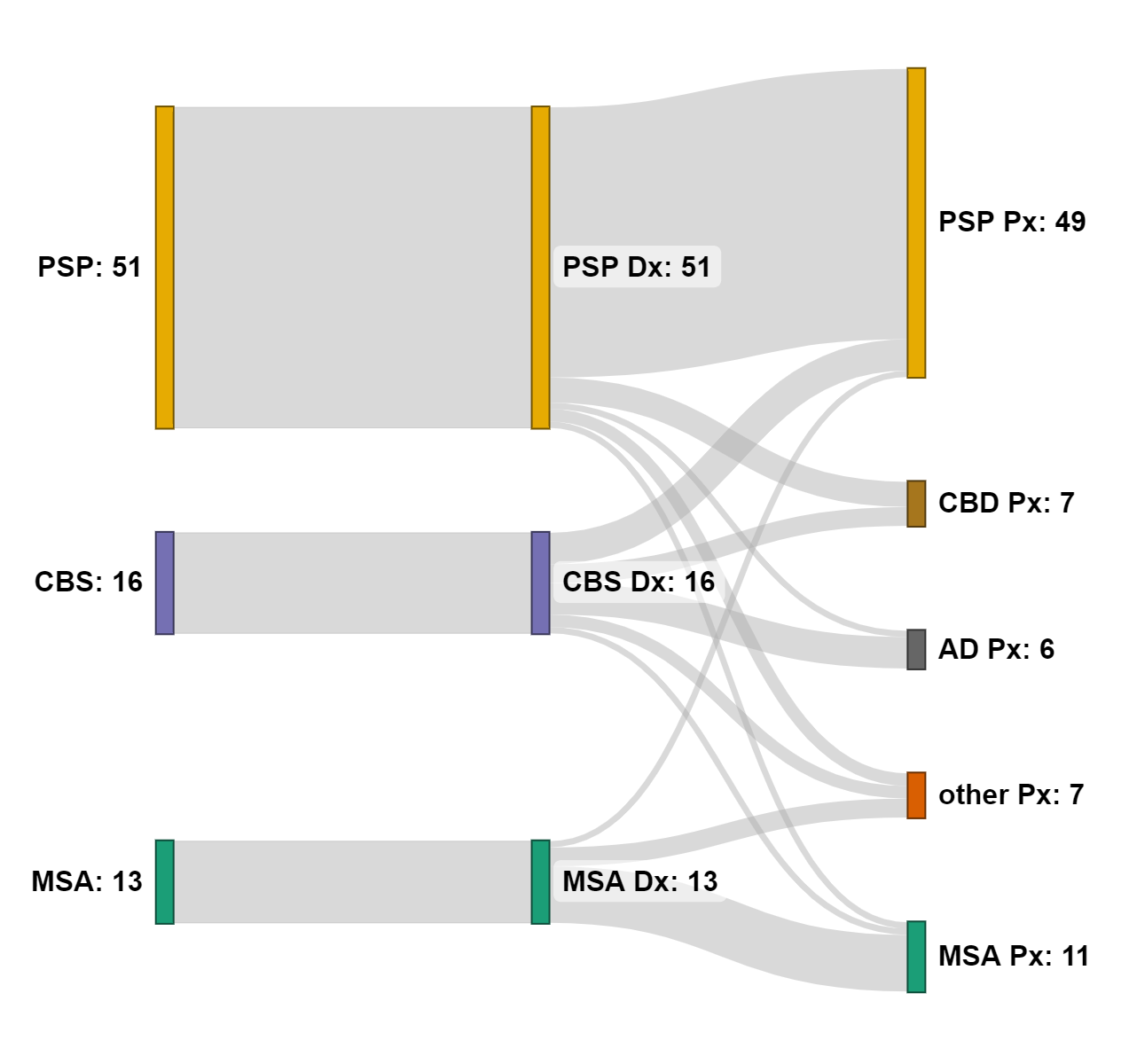
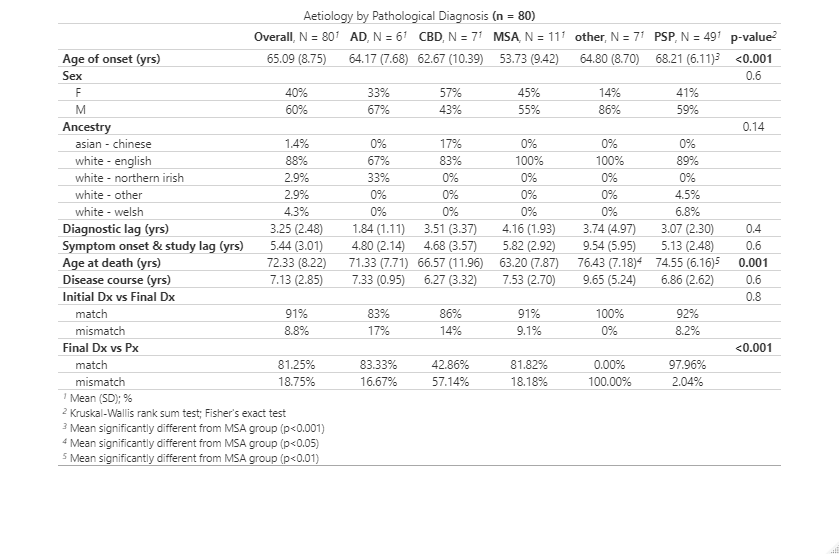
Results: Primary pathological diagnoses were PSP (n=49), corticobasal degeneration (CBD) (n=7), Alzheimer’s disease (AD) (n=6), MSA (n=11) and other pathologies (n=7) [figure1]. Clinical diagnosis was correct in 82.5% cases. Positive predictive value (PPV) was highest in PSP (84.3%) and lowest in MSA (69.23%). Diagnostic sensitivity was highest in PSP (87.75%) and lowest in CBS (72.2%). People with PSP were older (p<0.001) [table1] and had higher CBI scores than those with MSA (p<0.01). Those with underlying AD pathology were less likely to experience sleep problems (p<0.05). Generalised neuroparenchymal atrophy and cerebellar atrophy differed between 4R-taupotahies, amyloidopathies and synucleinopathies. Further analysis of imaging, genetics and biomarkers biomarkers is underway.
Conclusion: Diagnostic accuracy as confirmed at post-mortem is high for people with PSP. Patients with MSA are younger. Clinical scores from the CBI and UPDRS including non-motor experiences of daily living could be useful factors supporting specific diagnoses.
To cite this abstract in AMA style:
R. Fumi, M. Theilmann Jensen, L. Wu, D. Vaughan, V. Chelban, Y. Goh, R. Real, A. Martinez Carrasco, E. Jabbari, A. Church, J. Coebergh, C. Kobylecki, U. Nath, M. Hu, A. Misbahuddin, J. Sharma, L. Massey, E. Capps, A. Robinson, F. Roncaroli, A. Lees, O. Ansorge, K. Allison, T. Warner, J. Rohrer, T. Revesz, Z. Jaunmuktane, J. Rowe, H. Houlden, H. Morris. Clinico-pathological correlations in atypical parkinsonism [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/clinico-pathological-correlations-in-atypical-parkinsonism/. Accessed December 27, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinico-pathological-correlations-in-atypical-parkinsonism/