Category: Parkinson's Disease: Cognitive functions
Objective: To evaluate the relationship between sleep architecture and cognitive function in Parkinson disease (PD).
Background: About half of PD patients develop mild cognitive impairment within 6 years of diagnosis, (1) and up to 75% develop dementia after 10 years. (2) Disrupted sleep impacts cognition and is associated with an increased risk of dementia, (3) but its link to cognitive impairment in PD is poorly understood.
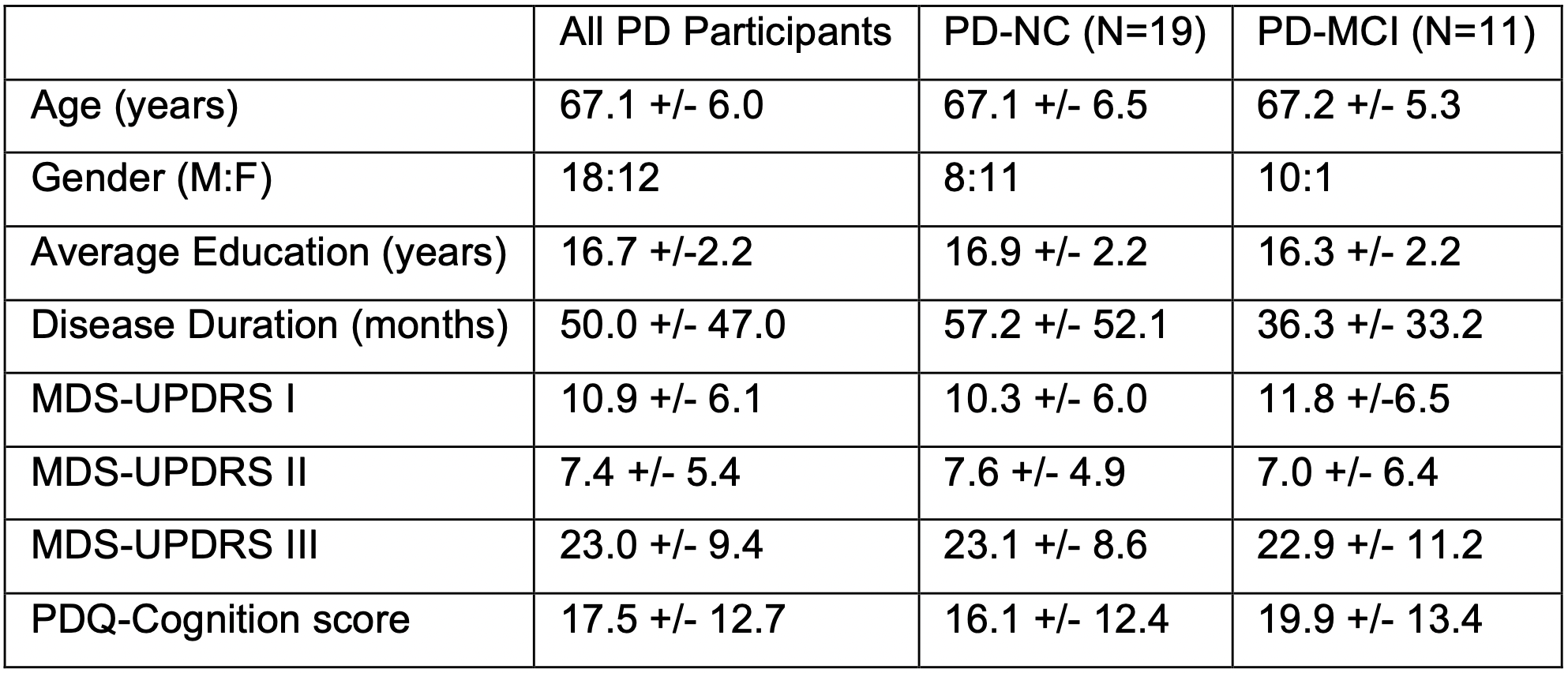
Method: Non-demented PD patients aged 50-80 were recruited. Patients were screened with the Montreal Cognitive Assessment (MoCA) and a full cognitive battery that included two tests in each cognitive domain: executive function, memory, language, attention/working memory, and visuospatial function. Patients were classified as PD-MCI if they scored 1.5 SD below the normative mean on at least two tests or had a MoCA<26. An overnight polysomnogram was used to estimate total sleep time (TST), sleep efficiency (SE), and total times in Rapid Eye Movement (REM) and non-REM (NREM) sleep. Additional clinical assessments included the MDS-UPDRS I-III and the Parkinson Disease Questionnaire (PDQ-39). Differences in sleep measures between PD with normal cognition (PD-NC) and PD-MCI were evaluated with t-tests. Sleep measure correlations with clinical assessments across the entire PD cohort were tested with Pearson correlation coefficients. Significance threshold was p<0.05.
Results: Thirty PD patients were included in our analysis (Table 1). Compared to PD-NC, PD-MCI had less TST (289.0±58.7 min vs 360.7±77.2 min, p=0.013) and NREM (197.2±100.7 min vs 282.6±78.2 min, p=0.015). TST was correlated with performance on immediate verbal recall (r=0.48, p=0.01) and delayed verbal recall (r=0.44, p=0.02). The total NREM time correlated with performance on immediate verbal recall (r=0.45, p=0.01), and negatively correlated with MDS-UPDRS I (r=-0.46, p=0.01). PDQ-39 cognitive domain scores negatively correlated with TST (r=-0.42, p=0.02), SE (r=-0.38, p=0.04), and total NREM time (r=-0.37, p=0.04). No significant correlations were found between sleep measures and motor symptoms (MDS-UPDRS II and III).
Conclusion: Total NREM duration is reduced in PD-MCI and this reduction may especially impair verbal memory and negatively impact non-motor symptom burden. Future study is needed to determine the biological variables that are relevant to these associations.
References: (1) Pigott K, Rick J, Xie SX, et al. Longitudinal study of normal cognition in Parkinson disease. Neurology. 2015;85(15):1276-1282. doi:10.1212/WNL.0000000000002001
(2) Aarsland D, Kurz MW. The epidemiology of dementia associated with Parkinson disease. J Neurol Sci. 2010 Feb 15;289(1-2):18-22. doi: 10.1016/j.jns.2009.08.034.
(3) Sabia, S., Fayosse, A., Dumurgier, J. et al. Association of sleep duration in middle and old age with incidence of dementia. Nat Commun 12, 2289 (2021). https://doi.org/10.1038/s41467-021-22354-2
To cite this abstract in AMA style:
S. Shah, C. Dintino, S. Lageman, N. Mukhopadhyay, E. Shelton, S. Holden, J. Broussard, L. Cloud, M. Barrett, B. Berman. Reduced non-REM sleep in Parkinson disease is associated with memory impairment and non-motor symptom burden [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/reduced-non-rem-sleep-in-parkinson-disease-is-associated-with-memory-impairment-and-non-motor-symptom-burden/. Accessed December 22, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/reduced-non-rem-sleep-in-parkinson-disease-is-associated-with-memory-impairment-and-non-motor-symptom-burden/