Objective: To assess the burden of access to diagnosis and botulinum neurotoxin (BoNT) treatment in Turkish patients with dystonia and hemifacial spasm (PwD/HFS).
Background: Diagnostic delays are common in PwD/HFS [1]. In addition, access to BoNT treatment is not widespread in Turkey. Optimizing healthcare in dystonia requires understanding patient experiences, which can be obtained using patient journey maps [2].
Method: Subjective experiences of PwD/HFS related to access to diagnosis and BoNT treatment were collected using a patient survey tailored to the Turkish healthcare system. Data were collected between October 2022 and March 2023 in seven university hospitals in seven regions of Turkey and were descriptively analyzed.
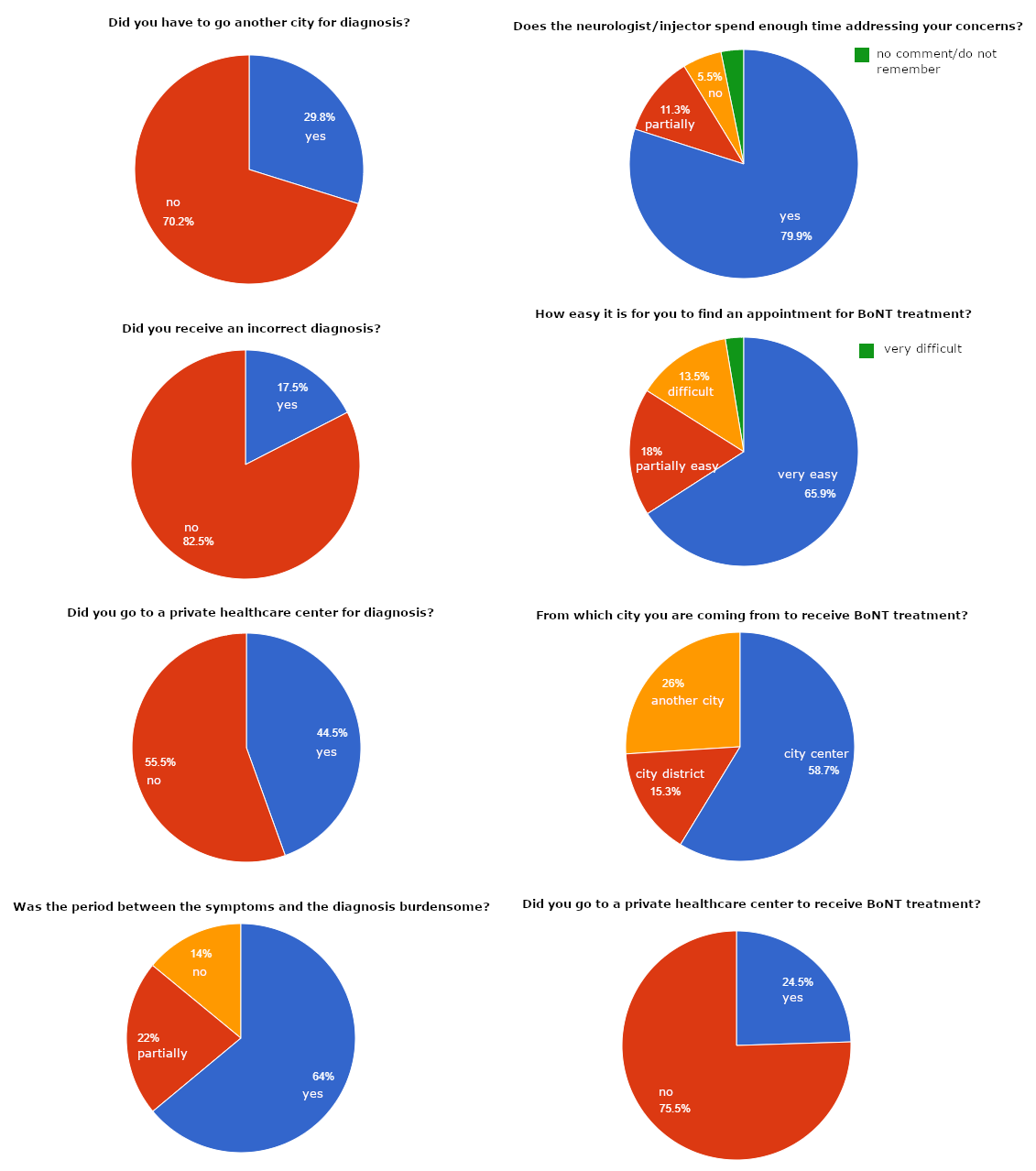
Results: A total of 622 PwD/HFS from 62 cities were enrolled in seven centers. The mean age was 56.7 (±14.7) and 66.9% were female. Of the included, 281 (45.2%) had cervical dystonia, 257 (41.3%) had blepharospasm or HFS, 41 (6.6%) had oromandibular dystonia, 34 (5.5%) had segmental or generalized dystonia, and nine (1.4%) had task-specific dystonia. The median values for symptom onset and diagnosis were 10 (IQR: 11), and 7 (IQR: 9) years ago, respectively, indicating a three-year delay in diagnosis which was reported as a burdensome period by 64% of PwD/HFS. In addition, 29.8% (n=187) of the PwD/HFS reported that they had to travel to another city for diagnosis. The frequency of incorrect diagnosis and treatment was 17.5%.
The first BoNT treatment was administered approximately two months after diagnosis. Around one-third (34.1%) stated that finding an appointment for BoNT treatment is challenging. In addition, 26% stated that they needed to travel to another city every three months to receive BoNT treatment which costs approximately 7.5% of their monthly household income. Almost all respondents (93.1%) stated that the neurologist/injector spent enough time addressing their concerns, and 93.6% were satisfied with BoNT treatment. However, 24.5% reported that they had to go to private clinics and pay for BoNT treatment at least once (figure-1).
Conclusion: The results suggest considerable regional inequality in the healthcare facilities for PwD/HFS. While PwD/HFS are satisfied with BoNT treatment, access to early and accurate diagnosis and BoNT treatment is challenging. Healthcare services should be reorganized considering the unmet needs of PwD/HFS.
References: [1] Bertram KL, Williams DR. Delays to the diagnosis of cervical dystonia. J Clin Neurosci 2016;25:62–4.
[2] Benson M, Albanese A, Bhatia KP, Cavillon P, Cuffe L, König K, et al. Development of a patient journey map for people living with cervical dystonia. Orphanet J Rare Dis 2022;17:1–9.
To cite this abstract in AMA style:
R. Yilmaz, N. öksüz, B. Samancı, A. Acarer, M. Ceylan, N. Durmaz-Celik, H. Erdem, S. özkan, H. Hanağası, O. Doğu, C. Akbostancı. Diagnostic and treatment burden of dystonia in Turkey: a patient journey map [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/diagnostic-and-treatment-burden-of-dystonia-in-turkey-a-patient-journey-map/. Accessed January 1, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/diagnostic-and-treatment-burden-of-dystonia-in-turkey-a-patient-journey-map/