Category: Parkinsonism, Atypical: MSA
Objective: SBD are frequent in MSA, mainly represented by inspiratory stridor, obstructive and central sleep apnea/hypopnea syndrome (SAS), or hypopneaimpacting the quality of sleep. A treatment withby CPAP can be proposed although but these its short-term and long-term effect on sleep architecture and breathing parameters remains unclear.
Background: SBD are frequent in MSA, mainly represented by inspiratory stridor, obstructive and central sleep apnea/hypopnea syndrome (SAS), impacting the quality of sleep. A treatment wtih CPAP can be proposed but its short-term effect on sleep architecture and breathing parameters is not fully understood.
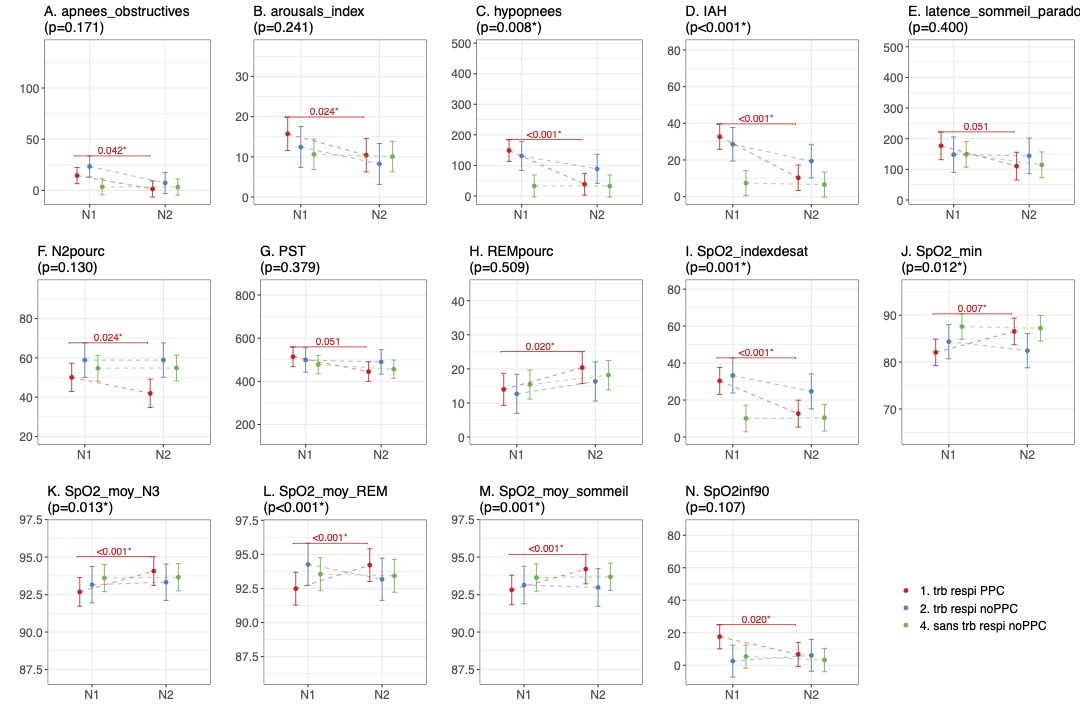
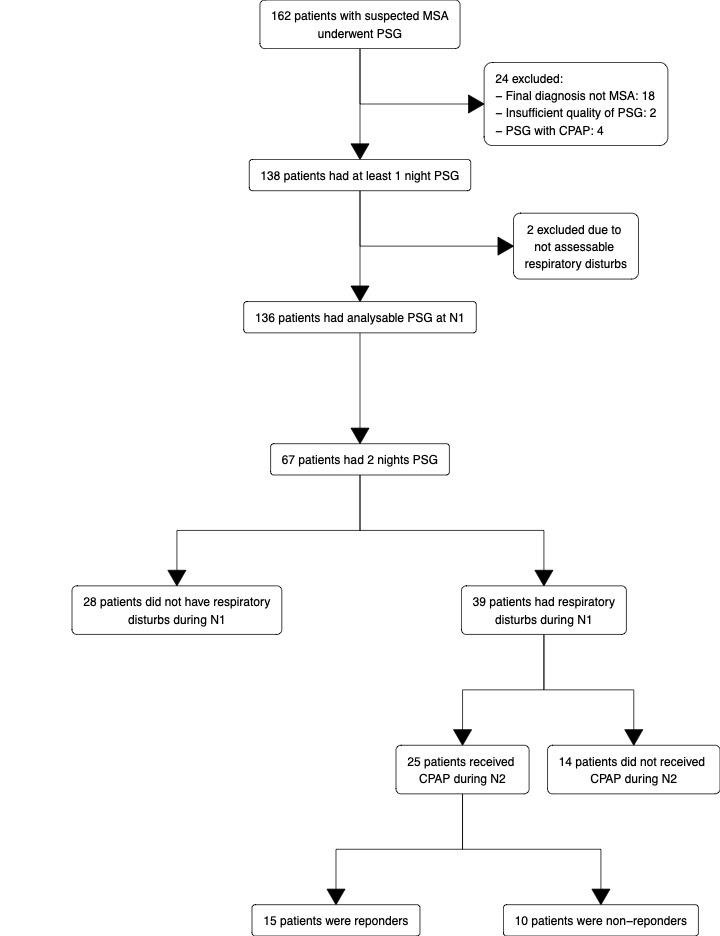
Method: Consecutive MSA patients with available data (n=67) recorded at the Sleep Unit of Pitié Salpêtrière Hospital, Paris, France, between April 2009 and July 2022 were included in the study. SDB was defined by the presence of stridor and/or apnea-hypopnea index (AHI)≥15 during the 1st night. We compared the clinical-demographic data (concomitant with PSG) between patients with and without SDB and the change in sleep parameters between the 2 nights in three groups: 1) with SDB and CPAP on the 2nd night 2) with SDB without CPAP, 3) without SDB, using linear mixed models. Group 1 patients were classified as responders to CPAP if on the 2nd night AHI was ≤10 and stridor was absent.
Results: SDB was present in 39/67 (58.2%) patients, 8 (20.5%) had isolated stridor, 16 (41.1%) SAS and 15 (38.4%) both. MSA-C patients were more often associated with SDB (64.1% vs 28.6%, p=0.006) compared to MSA-P patients. Patients with SDB had higher AHI (27.3 vs 2.5, p<0.001) and more fragmented sleep (median arousal index (AI) of 14.5 vs 7.5 (p=0.014)). After one night with CPAP, patients in group 1 had a decreased AHI (p<0.001), AI (p 0.024), and N2 stage duration (p=0.024) as well as an increased saturation in oxygen in all sleep stages (p<0.001) and REM sleep duration (p=0.020), whereas no evolution was found in both other groups. Among them, 15/25 (60 %) were responders, 3 (20%) with isolated stridor, 4 (26.7%) with SAS, 8 (53.3%) with both.
Conclusion: SDB is more frequent in MSA-C patients. We found a short-term effect of CPAP with better continuity in sleep and a rebound in REM sleep, as well as a good efficiency on SBD. Further studies exploring the value of this short-term response to predict the effect of CPAP on sleep quality over time are necessary.
To cite this abstract in AMA style:
G. Lazzeri, M. Houot, M. Patout, F. Cormier, M. Vidailhet, JC. Corvol, I. Arnulf, D. Grabli, P. Dodet. Short-term effect of continuous positive airway pressure in MSA patients with sleep disordered breathing [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/short-term-effect-of-continuous-positive-airway-pressure-in-msa-patients-with-sleep-disordered-breathing/. Accessed January 5, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/short-term-effect-of-continuous-positive-airway-pressure-in-msa-patients-with-sleep-disordered-breathing/