Category: Parkinsonism, Atypical: MSA
Objective: Presenting a case of Multiple System Atrophy (MSA) confirmed by skin biopsy with a peculiar genetic profile.
Background: MSA is a rare neurodegenerative disorder characterized by parkinsonism, autonomic failure, cerebellar and pyramidal signs, of unknown etiology and with a sporadic occurance occurrence, though in recent years several rare genetic variants have been reported associated to an increased risk of MSA
Method: Clinical examination, brain MRI, Real-Time Quaking Induced Conversion assay (RT-QuIC) and Immunohistochemical analysis (IHC) performed on skin biopsy; Simoa technology for blood neurofilament light chain (NfL).
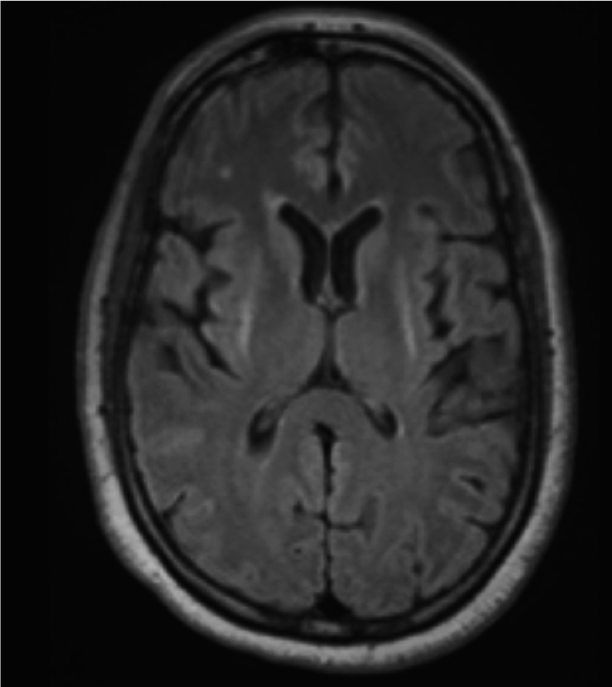
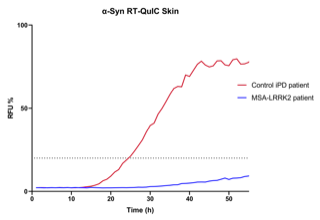
Results: We present the case of a North African woman with a rapidly progressive clinical picture characterized by dysautonomic features (urinary incontinence, orthostatic hypotension), poorly LDopa-responsive parkinsonism and eventually bulbar symptoms (stridor, dysphagia), for which she was diagnosed with MSA-p in her sixth decade. The typical neuroimaging findings supported the diagnosis: Dopamine Transported imaging (DAT-SPECT) demonstrated a severe reduction in the uptake of the tracer in the putamen bilaterally, whereas brain MRI showed bilateral slit-like hyperintensity on T2WI in the outer margin of the putamina and moderate putaminal atrophy. Genetic testing documented a single variant G2019S in leucine-rich repeat kinase 2 (LRRK2) gene. A skin biopsy was performed on the patient; the skin samples underwent alpha-synuclein RT-QuIC, that resulted negative, and IHC, which demonstrated abnormal alpha-synuclein deposits in cutaneous nerves. Elevated blood NfL levels were also detected.
Conclusion: LRRK2 mutations are the most common known causes of monogenic Parkinson’s disease (PD), with G2019S as its most frequent variant. Our patient presented with all the clinical and radiological features traditionally attributed to MSA, but genetic testing revealed a the G2019S LRRK2 mutation, which has been previously reported only in a single case of pathologically-proven MSA. In our case, post-mortem confirmation was not performed but RT-QuIC and ICH findings on skin biopsy supported the clinical diagnosis of MSA. Considering also the molecular effects induced by this mutation, our opinion is that G2019S LRRK2 could be linked to a higher risk of MSA and a worse prognosis, as witnessed by the rapid clinical progression and the high value of blood NfL reported in our case, but evidences still need to follow.
To cite this abstract in AMA style:
T. Carrer, G. Bonato, M. Sandre, A. Emmi, A. Antonini. LRRK2 G2019S mutation in Multiple System Atrophy, a case report [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/lrrk2-g2019s-mutation-in-multiple-system-atrophy-a-case-report/. Accessed April 1, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/lrrk2-g2019s-mutation-in-multiple-system-atrophy-a-case-report/