Category: Surgical Therapy: Parkinson's Disease
Objective: To test whether the length of the subthalamic nucleus (STN) in microelectrode recording (MER) can predict the 6-month motor and non-motor outcomes of DBS in Parkinson’s disease (PD).
Background: Two retrospective studies which tested the association of STN MER length and motor outcomes showed conflicting results.1,2 No previous study has tested STN length as a predictor of non-motor outcomes.
Method: Patients with PD who qualified for STN-DBS under MER (5-channel) and macrostimulation guidance, were prospectively enrolled. Pre-operative evaluation of UPDRS I to VI in drug ON and OFF states and non-motor evaluations using non-motor symptoms scale (NMSS), Parkinson’s disease fatigue scale (PFS- 16), Parkinson’s disease sleep scale (PDSS), King’s Parkinson’s disease pain scale (KPPS), Parkinson’s disease questionnaire (PDQ-39), Montreal cognitive assessment (MoCA), Frontal assessment battery (FAB) and Beck’s depression inventory (BDI) were performed. Intra-operative data of the number of MER electrodes used, number of STN tracks, and length of the final track used for lead implantation were recorded for each side. Follow-up evaluations were done in drug OFF, stimulation ON and drug OFF stimulation OFF (1 hour). The total electrical energy delivered (TEED) at 6 month visit was calculated [TEED = (voltage2 x pulse width x frequency)/ impedance]. Pearson’s correlation was used to test the association between the MER length and the motor and non-motor outcomes.
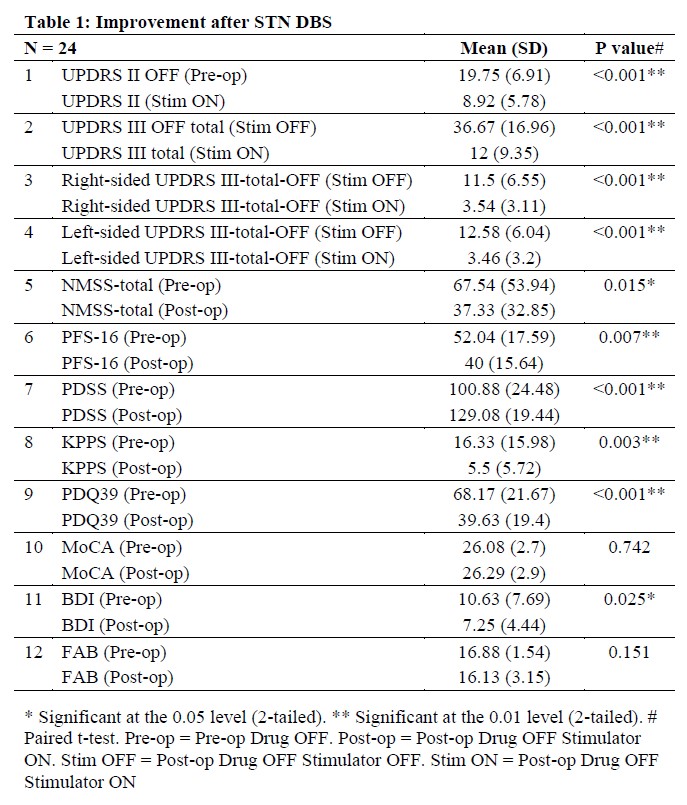
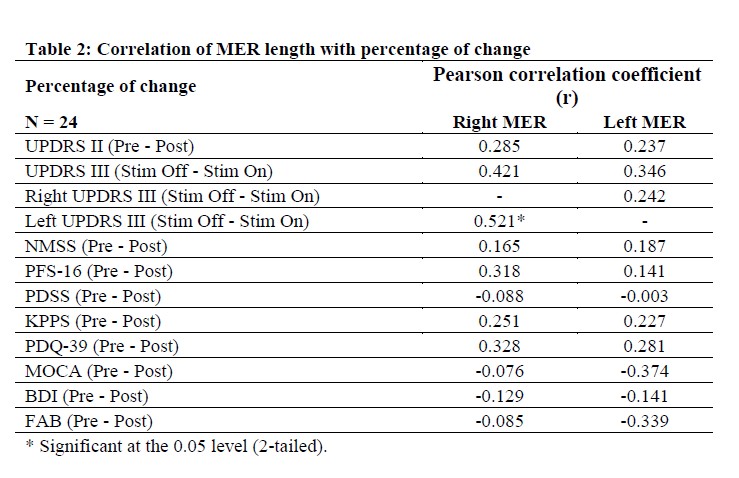
Results: 24 patients (mean age = 61 ± 8 years , mean duration of disease = 9.6 ± 4.8 years) completed 6-month assessments. The percentage changes are shown in Table 1. The mean length of STN in MER in the final track was 4.9 ± 1.4 mm on the right and 5.1 ± 1.5 mm on the left. The mean TEED was 33.2 ± 24.8 for the right and 39.9 ± 26.4 for the left. No significant association was found between the MER length or TEED with the motor and non-motor outcomes (Table 2).
Conclusion: Length of STN in MER does not predict either motor or non-motor outcomes of DBS. The choice of final track for lead placement based on stimulation thresholds for benefits and side effects may be preferred. The exact location of active electrode within the STN and the intensity of stimulation which optimally modifies the pathological electrical activity in the motor or non-motor circuits of STN may determine the outcome.
References: 1. Boëx C, Tyrand R, Horvath J, et al. What Is the Best Electrophysiologic Marker of the Outcome of Subthalamic Nucleus Stimulation in Parkinson Disease? World Neurosurg. 2018;120:e1217-e1224. doi:10.1016/j.wneu.2018.09.047
2. Shenai MB, Patel DM, Romeo A, et al. The Relationship of Electrophysiologic Subthalamic Nucleus Length as a Predictor of Outcomes in Deep Brain Stimulation for Parkinson Disease. Stereotact Funct Neurosurg. 2017;95(5):341-347. doi:10.1159/000478023
To cite this abstract in AMA style:
K. Pillai, S. Joshua, A. Nair, D. Panikar, M. Chacko, A. Thalakkattu, A. Avarachan, H. Prakash, A. Kishore. MER length as a predictor of motor and non-motor outcomes of STN DBS in Parkinson’s disease [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/mer-length-as-a-predictor-of-motor-and-non-motor-outcomes-of-stn-dbs-in-parkinsons-disease/. Accessed April 1, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/mer-length-as-a-predictor-of-motor-and-non-motor-outcomes-of-stn-dbs-in-parkinsons-disease/