Category: Parkinson's Disease: Cognitive functions
Objective: – To identify risk factors for postoperative delirium (POD) after deep brain stimulation (DBS) surgery
– To personalize and optimize perioperative management
Background: The main risk factors for cognitive decline after DBS in Parkinson’s disease (PD) are higher age and preoperative cognitive deficits (1). These are also the main risk factors for POD which, in turn, increases morbidity and mortality and long-term cognitive decline (2). POD after DBS was retrospectively reported to occur in 5,8 to 42,6% of PD patients (3).
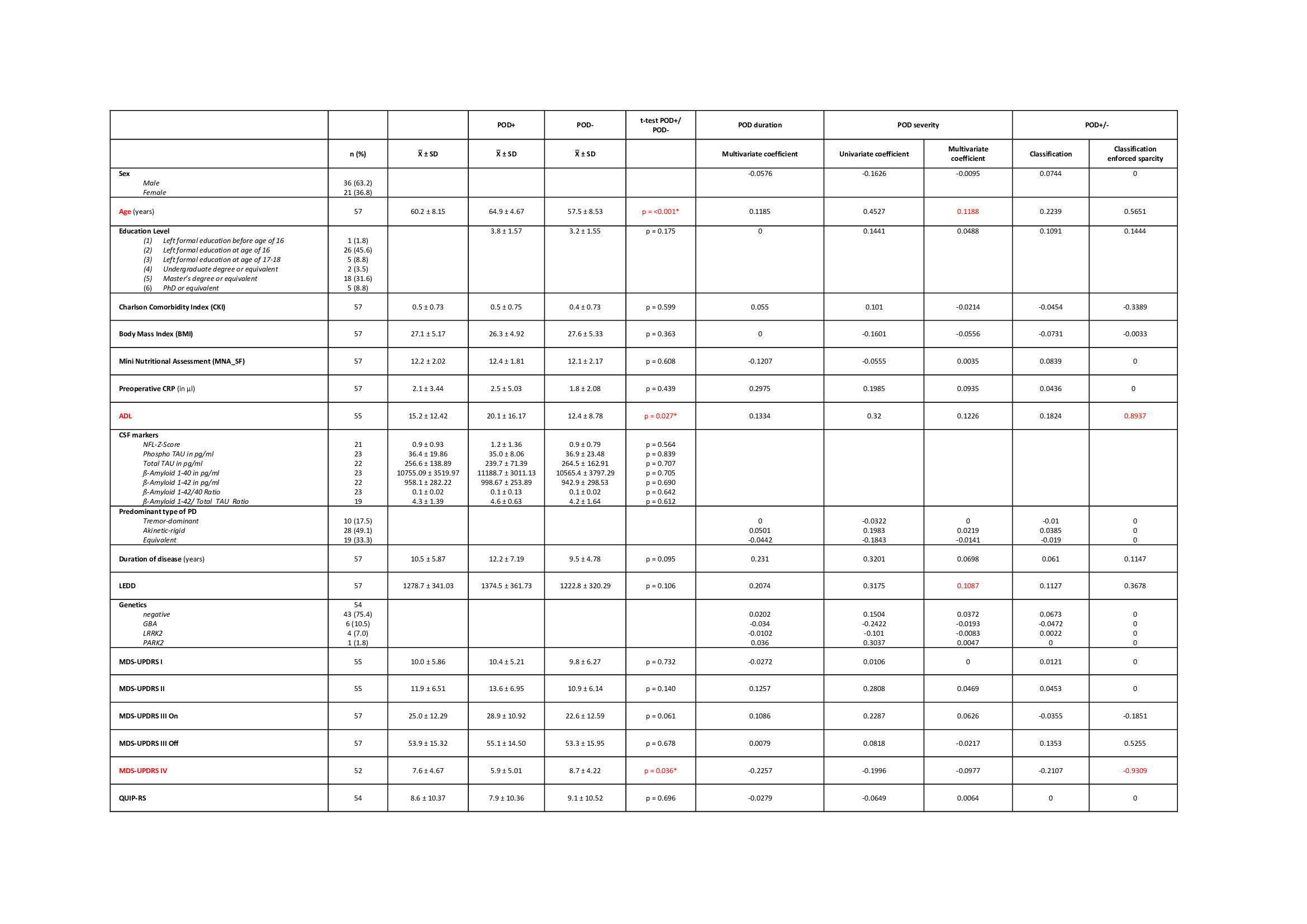
Method: 57 PD patients who underwent DBS surgery between 06/2019 and 09/2021 were included (21 female; Øage 60 (37-72); disease duration Ø10 (2-39) years). Preoperatively, the following possible predictors were recorded:
– General: Age, sex, education level, nutritional status, comorbidities, activity level, preoperative inflammation
– PD specific: Motor predominance type, PD duration, dopaminergic dose, MDS-UPDRS I-IV, PD-specific quality of life, depression, apathy, impulsive behaviors and PD specific gene mutations
– Cognition: Assessed with CANTAB Connect, a tablet-based neuropsychological examination, MoCA and a full neuropsychological examination
– Imaging: Volumes of the cholinergic basal forebrain (NBM and Ch1-3)
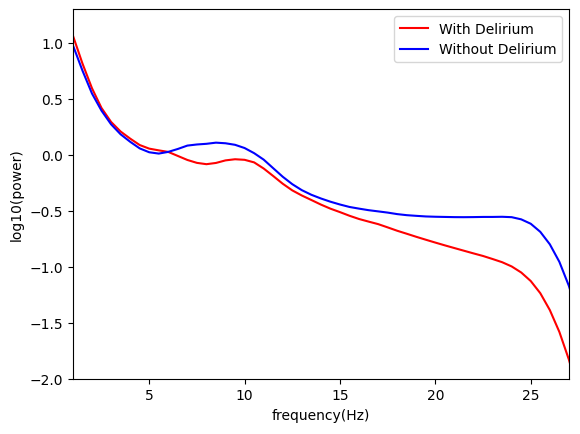
– Perioperative: Duration of dopaminergic pause, length of surgery, narcotics and depth of narcosis by frontal EEG (SedLine®).
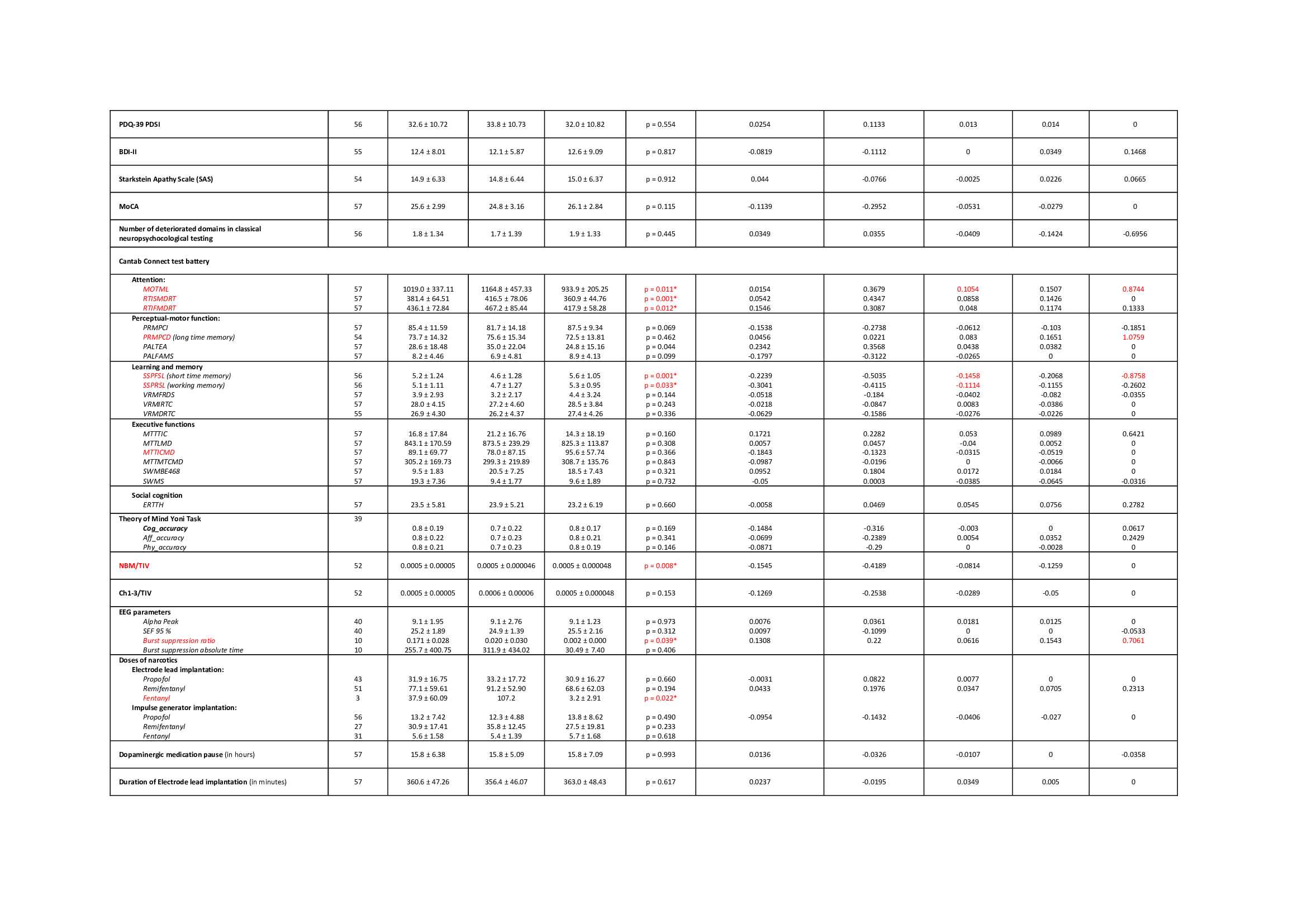
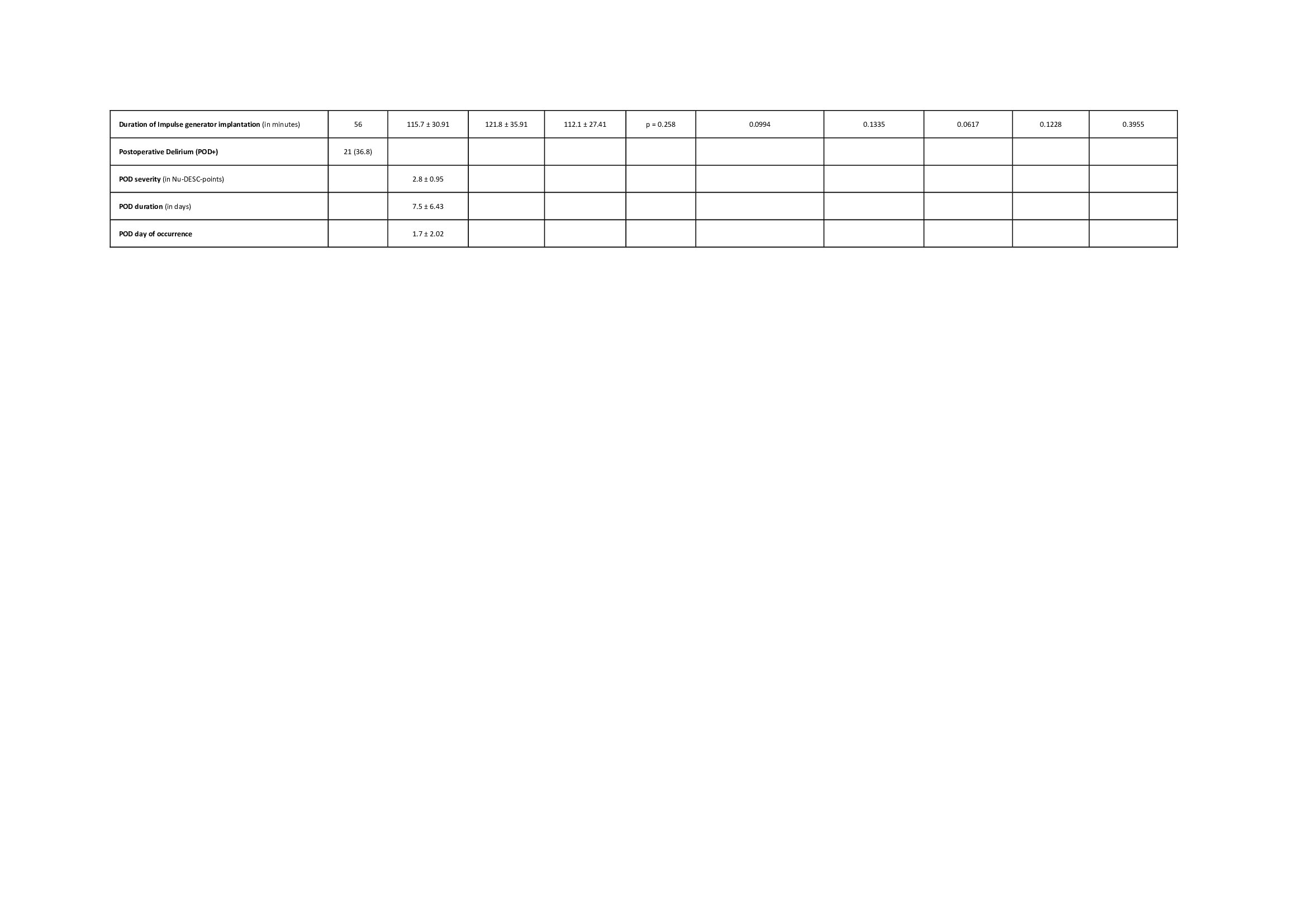
POD severity was recorded with validated scales (CAM-ICU/ Nu-DESC). To account for the high number and intercorrelation of possible predictors, we performed elastic net regularization and leave-one-out cross-validation to fit amultivariate model for prediction of POD after DBS surgery in PD.
Results: 21 (36,8%) patients showed a POD after DBS surgery (duration Ø7,5d (1-21), severity Ø2,8 Nu-DESC points (2-5,1). We found a significant correlation between predicted and true POD severity (Spearman rho=0.340, p=0.001). Multivariate coefficients of all predictors can be found in table 1. The most influential predictors were age, dopaminergic dose, short-time and working memory.
Conclusion: POD is common after DBS surgery. In our regularized regression model, both general and PD-specific factors were predictive of POD severity. We hope that our findings help clinicians to stratify perioperative management in order to gain optimal therapy outcomes.
References: 1. Maheshwary A, Mohite D, Omole JA, Bhatti KS, Khan S. Is Deep Brain Stimulation Associated With Detrimental Effects on Cognitive Functions in Patients of Parkinson’s Disease? A Systematic Review. Cureus. 2020;12(8):e9688.
2. European Society of Anaesthesiology. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Europe: Eur J Anaesthesiol; 2017 Apr. 192-214 p.
3. Li H, Han S, Feng J. Delirium after Deep Brain Stimulation in Parkinson’s Disease. Parkinsons Dis. 2021;2021:1-9.
To cite this abstract in AMA style:
M. Astalosch, M. Mousavi, L. Martins Ribeiro, GH. Schneider, H. Stuke, S. Haufe, F. Borchers, C. Spies, J. von Hofen-Hohloch, B. Al-Fatly, G. Ebersbach, C. Franke, A. Kühn, D. Kübler-Weller. Prediction of postoperative delirium after deep brain stimulation surgery in Parkinson`s disease [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/prediction-of-postoperative-delirium-after-deep-brain-stimulation-surgery-in-parkinsons-disease/. Accessed December 15, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/prediction-of-postoperative-delirium-after-deep-brain-stimulation-surgery-in-parkinsons-disease/