Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To investigate frequency of PD patients with symptoms of drooling and their clinical characteristics in our Japanese Parkinson’s disease (PD) registry data.
Background: Drooling directly affects the patient’s quality of life (QOL) by interfering with eating and speaking and causing emotional distress such as embarrassment. Drooling may also put patients at risk for aspiration pneumonia, which may have a life-threatening impact on their prognosis. However, the attention and care of healthcare providers and caregivers to drooling has been insufficient.
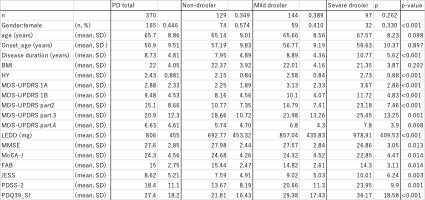
Method: The authors used registry data created for PD patients who were clinically established PD or clinically probable PD during the period between July 2019 and August 2022. We included population from whom those who had deficiencies in the drooling questionnaire (MDS-UPDRS Part II.2) and those under 40 years of age were excluded. Those who answered “normal” for saliva and drooling in MDS-UPDRS Part II.2 were classified as “non-droolers,” those who answered “very mild” or “mild” were classified as “mild droolers,” and those who answered “moderate” or “severe” were classified as “severe droolers”. A cross-sectional analysis was performed on these three stratified groups for gender, age, disease duration, age of onset, Hoehn & Yahr Stage, LEDD (Levodopa equivalent daily dose) and BMI, as well as for their motor symptoms, cognitive function, quality of life, and sleep symptoms.
Results: A total of 370 patients were included in the analysis. Their clinical characteristics are shown in Table 1. There were 129 (34.9%) patients in the non-drooling group, 144 (38.9%) patients in the mild drooling group, and 97 (26.1%) patients in the severe drooling group. The group of patients with drooling had significantly longer disease duration and higher Yahr severity, and the rate of male was higher than female in this group. They also presented significantly higher scores on the MDS-UPDRS Part I, Part II, Part III, and Part IV. MMSE, MoCA-J and FAB were performed to assess their cognitive functions, and the scores were were significantly low in all of them. Moreover, daytime sleepiness was significantly frequent, and sleep and quality of life were significantly low.
Conclusion: PD patients with drooling had more severe motor symptoms and non-motor symptoms than those without drooling did. Drooling is an important predictive clinical biomarker of disease severity in PD.
To cite this abstract in AMA style:
N. Nishikawa, E. Ikami, H. Takeshige, T. Ogawa, T. Hatano, N. Hattori. Drooling is associated with disease severity in Parkinson’s disease [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/drooling-is-associated-with-disease-severity-in-parkinsons-disease/. Accessed February 5, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/drooling-is-associated-with-disease-severity-in-parkinsons-disease/