Objective: To identify the effect of rasagiline on nocturnal hypokinesia based on Nocturnal Hypokinesia Questionnaire (NHQ).
Background: Nocturnal hypokinesia refers to the difficulty or the inability to turn in bed and get out of bed at night or in the morning. It is one of the significant disabling problems in PD patients and older adults in general. The clinical presentations of nocturnal hypokinesia can manifest as a difficult axial rotation during the night and during the getting up period, particularly during the early morning off period. Nocturnal hypokinesia is considered the longest wearing-off in PD and correlates with the daytime wearing-off symptoms. Rasagiline is one of the drugs of choice for the wearing-off treatment strategy. Unfortunately, the current effective treatment guideline for nocturnal hypokinesia was limited.
Method: The electronic form of the Nocturnal Hypokinesia Questionnaire (NHQ) was distributed via the Line official account (Line OA) of ChulaPD during the COVID 19 pandemic (Jan – Dec 2021). The members of the Line OA were PD patients and caregivers from our center. The demographic data also were collected.
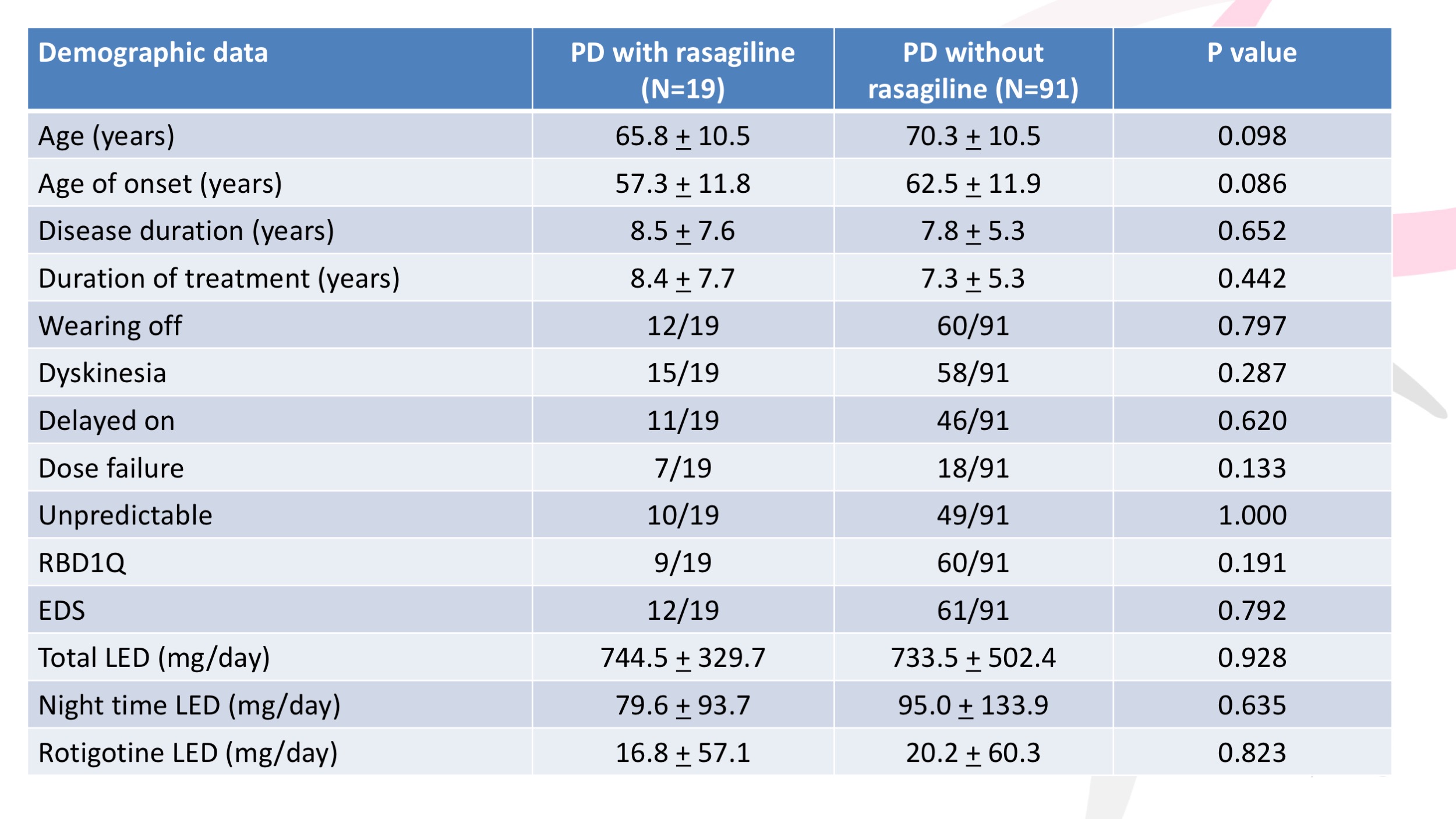
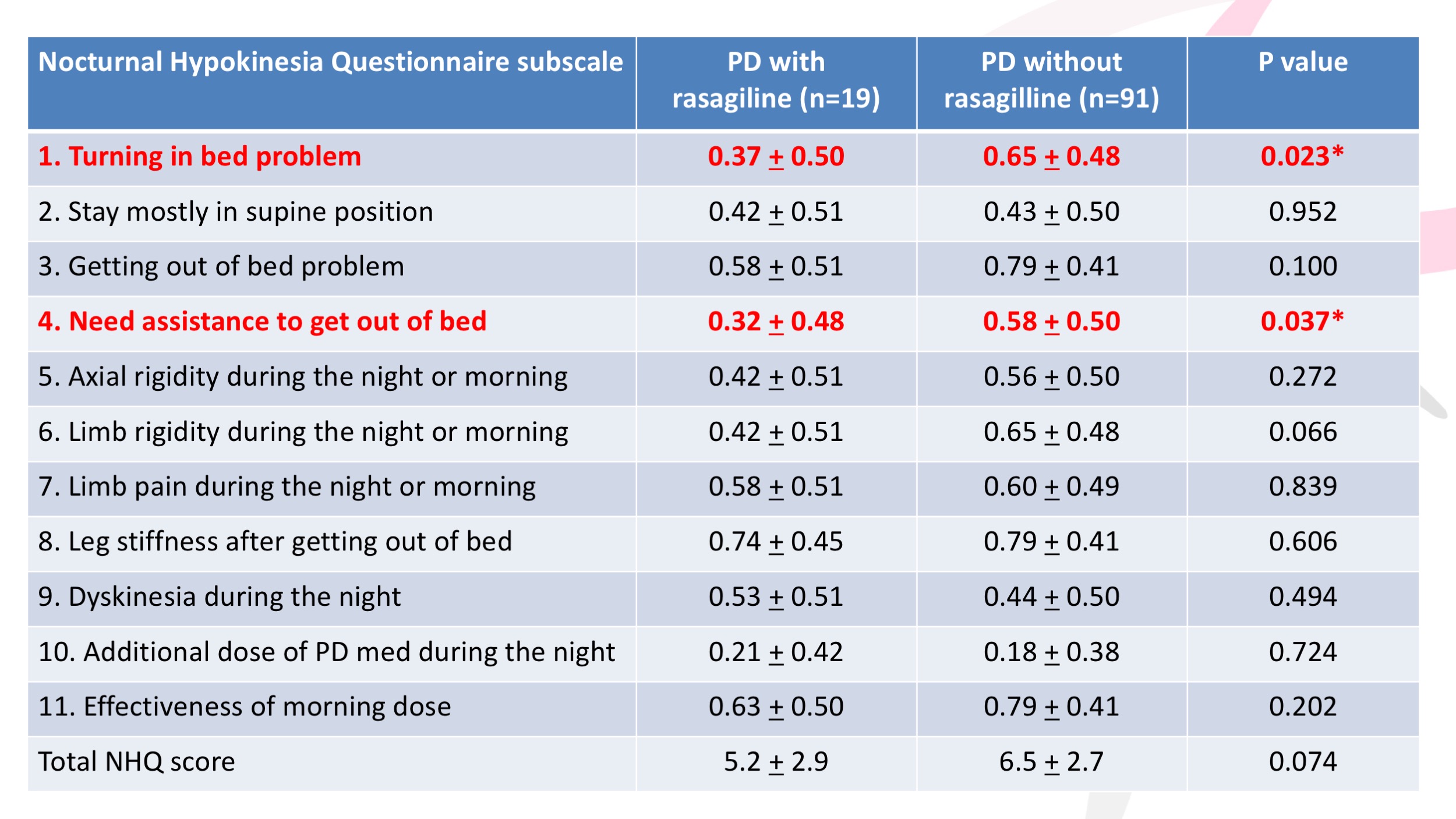
Results: 128 PD patients answered the electronic form of NHQ but 17 patients were dropped out from the analysis because of incomplete data. 19 PD were PD with rasagiline used and 91 PD were PD without rasagiline used. The mean age, age of onset, disease duration, and total LED dose were 65.8 + 10.5 vs 70.3 + 10.5 years, 57.3 + 11.8 vs 62.5 + 11.9 years, 8.5 + 7.6 vs 7.8 + 5.3 years, and 744.5 + 329.7 vs 733.5 vs 502.4 mg/day, respectively. The mean rasagiline equivalent dose in PD with rasagiline used was 86.8 + 22.6 mg/day. Other demographic data was shown in table 1. The total NHQ score in PD with rasagiline and without rasagiline were 5.2 + 2.9 vs 6.5 + 2.7, p-value 0.074. We found a statistically significant difference in item 1 (turning in bed problem) 0.37 + 0.50 vs 0.65 + 0.48, p-value 0.023 and item 4 (need assistance to get out of bed) 0.32 + 0.48 vs 0.58 + 0.50, p-value 0.037. Other items of NHQ were shown in table 2.
Conclusion: We found that the PD with rasagiline used had less turning in bed problems and need assistance to get out of bed than PD without rasagiline. These findings reviewed the effect of rasagiline as the treatment of nocturnal hypokinesia which is the longest wearing off period. Further study should be done.
References: 1. Bhidayasiri R, Sringean J, Trenkwalder C. Mastering nocturnal jigsaws in Parkinson’s disease: a dusk-to-dawn review of night-time symptoms. J Neural Transm (Vienna) 2020;127:763-77.
2. Sringean J, Taechalertpaisarn P, Thanawattano C, Bhidayasiri R. How well do Parkinson’s disease patients turn in bed? Quantitative analysis of nocturnal hypokinesia using multisite wearable inertial sensors. Parkinsonism Relat Disord 2016;23:10-6.
3. Bhidayasiri R, Sringean J, Thanawattano C. Sensor-based evaluation and treatment of nocturnal hypokinesia in Parkinson’s disease: An evidence-based review. Parkinsonism Relat Disord 2016;22 Suppl 1:S127-33.
4. Hattori N, Takeda A, Takeda S, Nishimura A, Kato M, Mochizuki H, Nagai M, Takahashi R. Efficacy and safety of adjunctive rasagiline in Japanese Parkinson’s disease patients with wearing-off phenomena: A phase 2/3, randomized, double-blind, placebo-controlled, multicenter study. Parkinsonism Relat Disord. 2018 Aug;53:21-27. doi: 10.1016/j.parkreldis.2018.04.025. Epub 2018 Apr 27. PMID: 29748109.
To cite this abstract in AMA style:
J. Sringean, R. Bhidayasiri. The effect of rasagiline on nocturnal hypokinesia: the analysis of the Nocturnal Hypokinesia Questionnaire (NHQ) [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/the-effect-of-rasagiline-on-nocturnal-hypokinesia-the-analysis-of-the-nocturnal-hypokinesia-questionnaire-nhq/. Accessed December 31, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-effect-of-rasagiline-on-nocturnal-hypokinesia-the-analysis-of-the-nocturnal-hypokinesia-questionnaire-nhq/