Category: Surgical Therapy: Parkinson's Disease
Objective: To describe the relation between the topography of subthalamotomy by focused ultrasound (FUS) for the treatment of Parkinson’s disease (PD) (1), and the risk of dyskinesias.
Background: One of the main concerns of subthalamotomy in PD patients is the occurrence of hemichorea-ballism. Evidence from radiofrequency suggests that impacting onto the dorsal subthalamic area provides a pallidotomy-like effect reducing the risk of subthalamotomy-induced dyskinesias.[2]
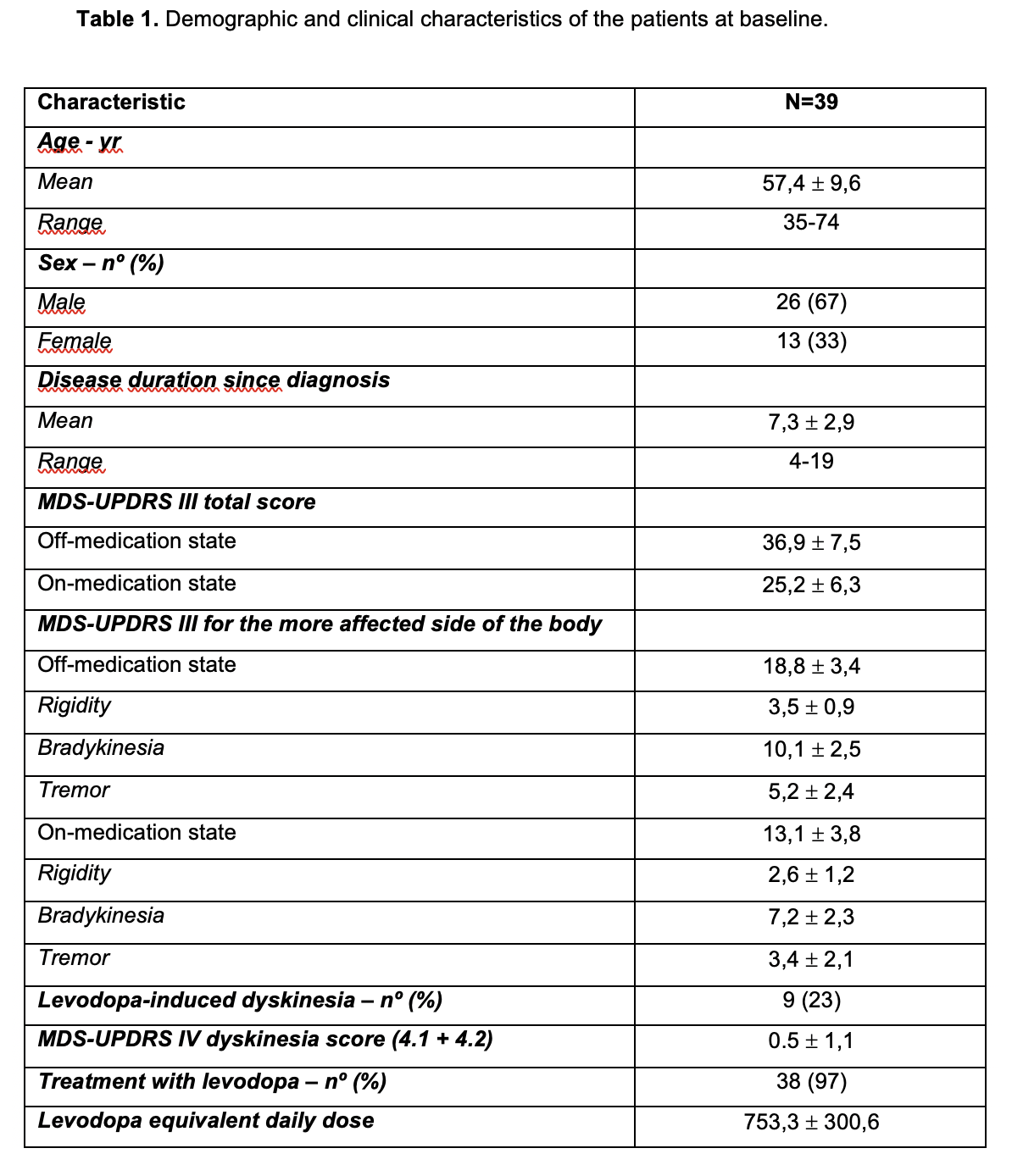
Method: We ascertained 39 patients treated with FUS unilateral subthalamotomy (Table 1), The relationship between topography of the lesion and incidence of dyskinesias. T1/T2 MR(3T) images at 24-hours post-procedure were used for analysis. Dyskinesias were evaluated clinically and according to patients´ report throughout 12 months follow-up. Dyskinesias were classified per intensity and location in their peak severity.
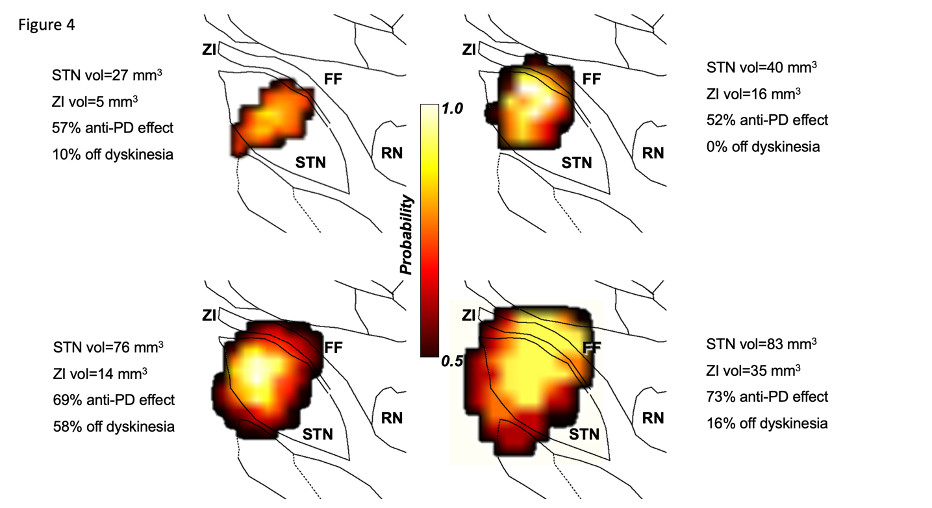
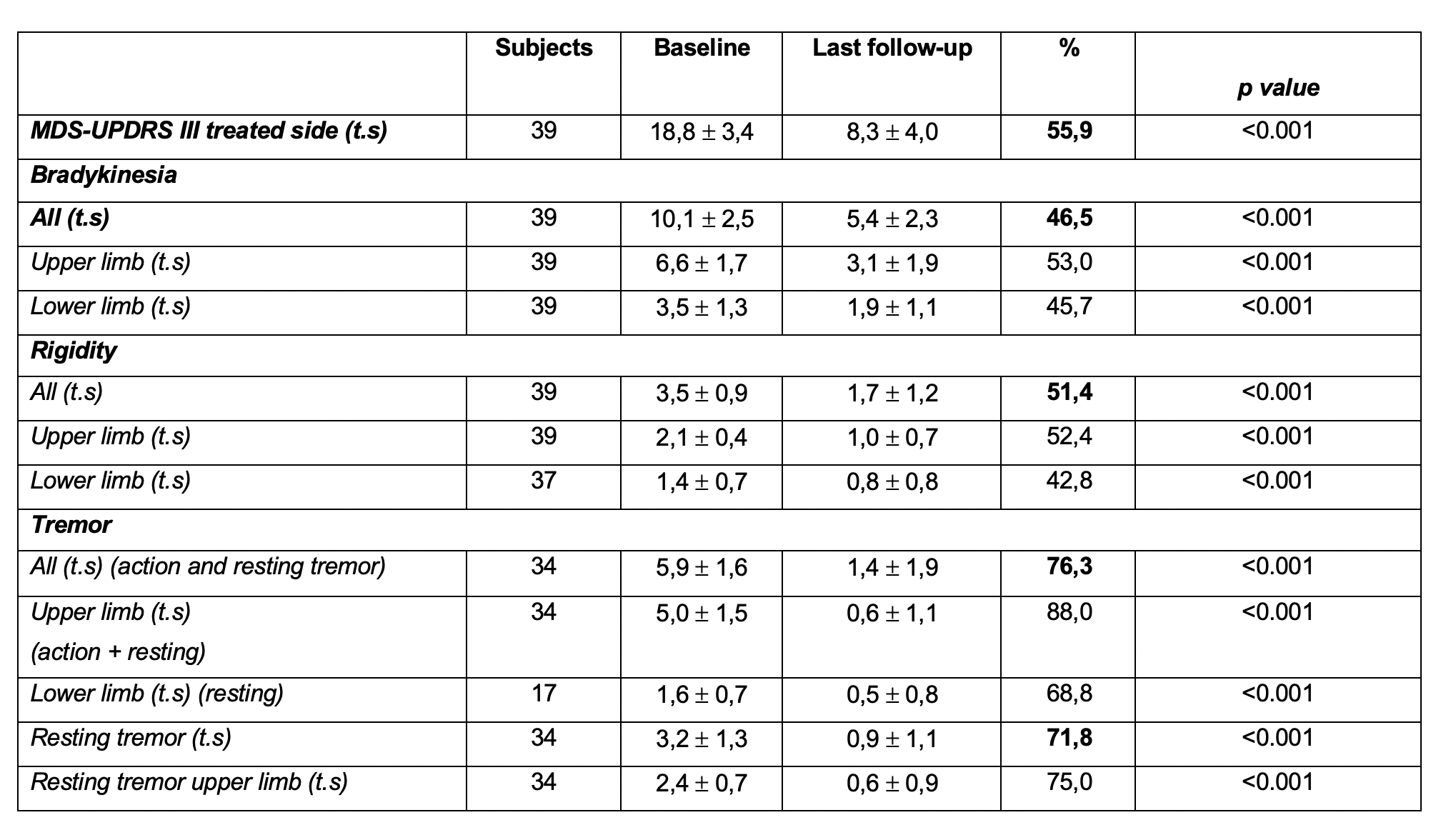
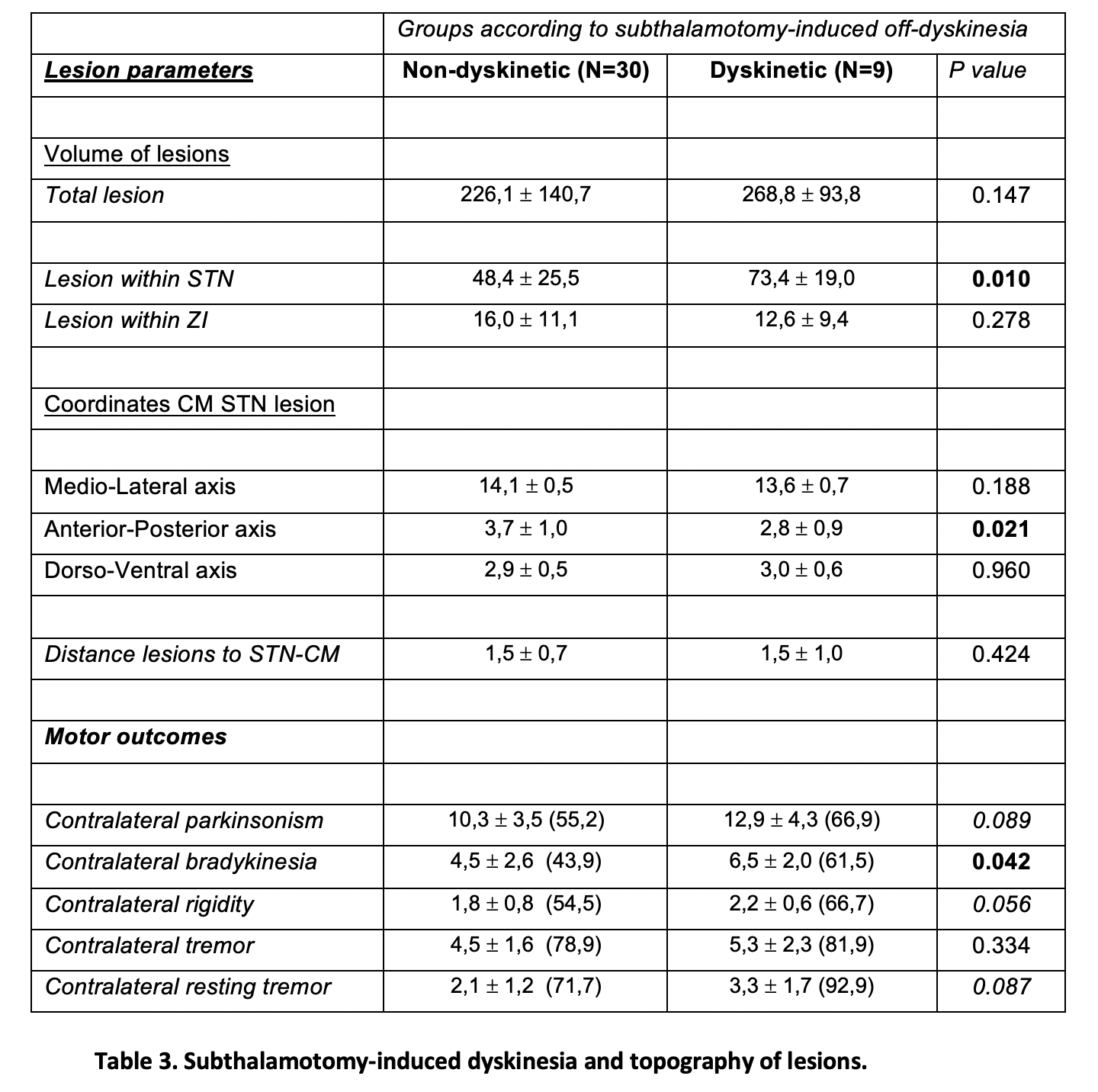
Results: Improvement in the off MDS-UPDRS-III on the treated side was 55.9% (Table 2). Lesions were located within the subthalamic area with a total volume of 235,9 ± 131,5 mm3. Impact within the STN accounted for 54,2 ± 26,2 mm3 in the motor region and lesions further enlarged dorsally into Forel Fields for a mean volume of 15,2 ± 10,7 mm3. Nine patients (23%) developed subthalamotomy-induced off-dyskinesia within the first few (1-7) days post-procedure. In all patients these vanished within the next six months. A principal component analysis showed four clusters and suggested that antiparkinsonian effect and risk of developing off-dyskinesias relayed on the relative balance between impacting on the STN proper and the pallido-fugal fibers (Figure 1) . Noteworthy, development of off-dyskinesia (n=9) was related with rostral lesions compared with non-dyskinetic subjects (n=30) and greater impact within the STN (Table 3).
Conclusion: Subthalamotomy exhibited a 23% incidence of dyskinesia. Evolution was positive in all cases at follow-up without any further complication. Lesions located rostrally within the STN with lesser impact on the palidofugal fibers have the highest risk of inducing chorea-ballism.
References: 1. Martínez-Fernández R, Rodríguez-Rojas R, Máñez-Miró JU, et al. Focused ultrasound subthalamotomy in patients with asymmetric Parkinson’s disease: a pilot study. Lancet Neurol. 2018;17(1):54–63. doi:10.1016/S1474-4422(17)30403-9.
2. Rodriguez-Rojas R, Carballo-Barreda M, Alvarez L, et al. Subthalamotomy for Parkinson’s disease: clinical outcome and topography of lesions Journal of Neurology, Neurosurgery & Psychiatry 2018;89:572-578.
To cite this abstract in AMA style:
J. Máñez-Miró, R. Rodríguez-Rojas, J. Pineda-Pardo, M. Del álamo, R. Martinez-Fernandez, J. Obeso. Relationship between lesion topography and incidence of dyskinesias following focused ultrasound subthalamotomy. [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/relationship-between-lesion-topography-and-incidence-of-dyskinesias-following-focused-ultrasound-subthalamotomy/. Accessed December 29, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/relationship-between-lesion-topography-and-incidence-of-dyskinesias-following-focused-ultrasound-subthalamotomy/