Objective: Neuropsychiatric symptoms (NPS) are closely associated with cognitive decline in patients with Parkinson’s disease (PD). We investigated which baseline profile of NPS predicts the risk of developing dementia in early-stage PD.
Background: Parkinson’s disease dementia (PDD) is one of the most important non-motor symptoms and affects the majority of PD patients in the advanced stage. As physical and cognitive disability increase with PDD conversion, identification of the risk factors for the development of dementia is important in the early stages of PD. Ample evidence suggests that NPS are closely associated with cognitive decline in patients with PD. However, since most studies identified the role of NPS in cognitive decline by employing specific NPS, or in pre-defined categorizations of NPS, this approach can be biased depending on the NPS selected.
Method: We retrospectively reviewed the medical records of 482 drug-naïve patients with PD without dementia who underwent a neuropsychiatric inventory (NPI) questionnaire. We conducted a factor analysis of 12 NPI symptoms, yielding four NPS factors: Factor 1, depression, anxiety, apathy, aberrant motor behavior, and eating change; Factor 2, aggression/agitation, disinhibition, and irritability; Factor 3, euphoria, and nighttime behavior; Factor 4, delusion, and hallucination. Subsequently, we evaluated the effect of NPS prevalence and severity factor scores on the risk and timing of PDD conversion. Additionally, we examined the putative interaction effect between NPS and sex on PDD conversion.
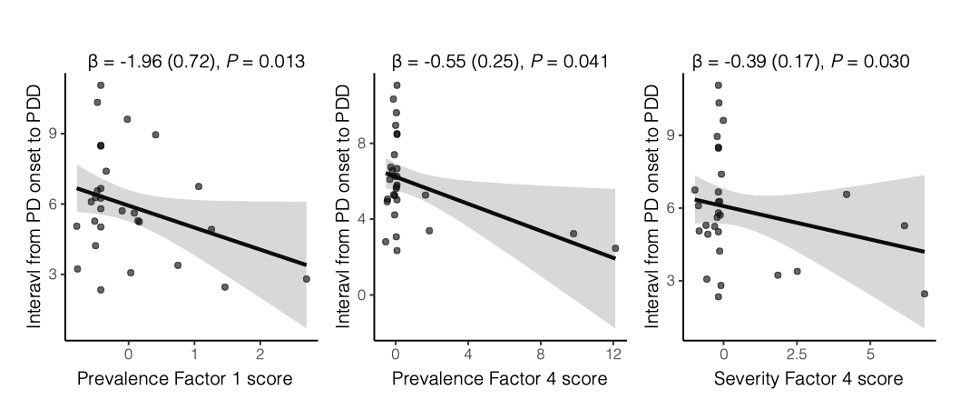
Results: In Cox regression analysis demonstrated that more prevalent NPS of Factor 2 (hazard ratio [HR] 1.13, 95% confidence interval [CI] 1.00–1.28) and more severe NPS of Factor 4 (HR 1.23, 95% CI 1.04–1.45) correlated with dementia conversion. In subgroup analysis according to sex, the relationship between the NPS factor scores and PDD conversion was only significant in male PD patients. The more prevalent NPS of Factors 2 (p = 0.01) and 4 (p = 0.04), and more severe NPS of Factor 4 (p = 0.03) correlated with early PDD conversion in male patients.
Conclusion: This study demonstrates the sex-specific effect of hyperactivity and psychosis symptoms on the PDD risk.
To cite this abstract in AMA style:
Y. Lee, SW. Kang, SH. Yoon, K. Baik, HK. Na, YH. Sohn, PH. Lee. Sex-specific factor analysis-derived profile of neuropsychiatric symptoms predicting dementia conversion in Parkinson’s disease [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/sex-specific-factor-analysis-derived-profile-of-neuropsychiatric-symptoms-predicting-dementia-conversion-in-parkinsons-disease/. Accessed April 2, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/sex-specific-factor-analysis-derived-profile-of-neuropsychiatric-symptoms-predicting-dementia-conversion-in-parkinsons-disease/