Category: Neuroimaging (Non-PD)
Objective: We present a patient with GAD65-Ab-related encephalomyelitis who developed unilateral hypertrophic olivary degeneration (HOD) in the absence of structural lesions within the Guillain-Mollaret triangle.
Background: Neuroimaging in syndromes associated with GAD65-Ab are usually either unremarkable or can show mesial temporal lobe T2-hyperintensities; in the cases of long-term predominant ataxia, cerebellar atrophy can be found [1].
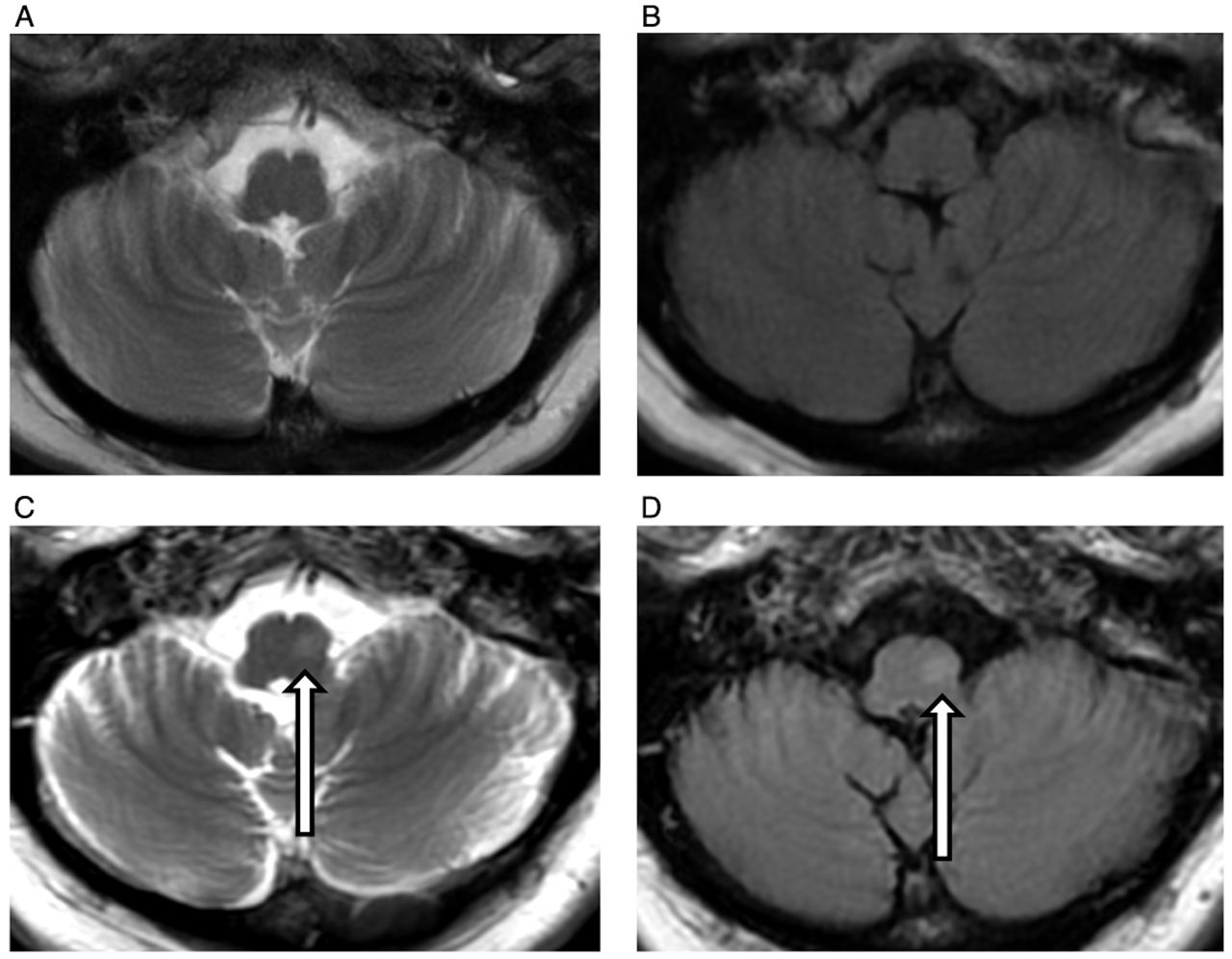
Method: A 55-year-old woman presented with stiffness of axial muscles, cerebellar syndrome, oculomotor abnormalities, and palatal tremor. At 32, she developed progressive stiffness in the abdomen muscles and episodic falls. At 43, she started experiencing episodic stiffening of the right leg, painful nocturnal muscle spasms, gait impairment, and diplopia. At 49, she was diagnosed with stiff person syndrome based on high serum GAD65-Ab titer (> 2000 U/mL) and continuous paraspinal muscle activity on EMG. Brain MRI was unremarkable. Clonazepam provided modest improvement; she refused oral steroids. At 53, 1st session of plasma exchange (PE) with a good clinical response for one year. She then started to use a walker and developed a skew deviation. Repeated PE led to no benefits. In March 2020, she received 3 g of IV methylprednisolone and 2 g/kg of IVIG, with improvement in eye movements, muscle stiffness, and gait. In August 2020, muscle stiffness and cerebellar ataxia worsened (patient lost ability to ambulate), and mild palatal tremor was found. Repeated 1.5T brain MRI showed left HOD with no lesions within the dentato-rubro-olivary pathway (Figure 1 C,D).
Results: Palatal tremor is a known rare symptom of the GAD65-Ab-related conditions [2], and HOD was not reported until recently [3,4]. In our patient, 1.5T brain MRI showed no brainstem lesions, suggesting functional chemical denervation as a possible cause of the unilateral HOD. Another explanation may be resolution limitations of a 1.5T MRI, as it was the case where 7T brain MRI allowed to identify only one causal lesion in a patient with bilateral HOD due to GAD65-Ab, and authors suggested that chemical denervation accounted for the hypertrophic degeneration of another inferior olive [3].
Conclusion: HOD may develop not only due to organic but also due to the functional disruption of the dentato-rubro-olivary pathways. GAD65-Ab-related neurologic disorders should be considered in the differential diagnosis in patients with HOD.
References: [1] Dade M, Berzero G, Izquierdo C, Giry M, Benazra M, Delattre J-Y, et al. Neurological Syndromes Associated with Anti-GAD Antibodies. Int J Mol Sci 2020;21:3701. https://doi.org/10.3390/ijms21103701.
[2] Nemni R, Braghi S, Natali-Sora MG, Lampasona V, Bonifacio E, Comi G, et al. Autoantibodies to glutamic acid decarboxylase in palatal myoclonus and epilepsy. Ann Neurol 1994;36:665–7. https://doi.org/10.1002/ana.410360419.
[3] Macaron G, Willis MA, Ontaneda D, Fernandez H, Kim S, Jones SE, et al. Palatal myoclonus, abnormal eye movements, and olivary hypertrophy in GAD65-related disorder. Neurology 2020;94:273–5. https://doi.org/10.1212/WNL.0000000000008926.
[4] Ip M, Li S, Wai T, Wong L. Oculopalatal tremor (OPT) in a patient with anti-GAD brainstem encephalitis: A case report [abstract]. Mov Disord 2019;34 (suppl.)
To cite this abstract in AMA style:
O. Turgunkhujaev, YU. Seliverstov, V. Fominykh, L. Brylev. Unilateral Hypertrophic Olivary Degeneration in Anti-GAD-associated Encephalomyelitis [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/unilateral-hypertrophic-olivary-degeneration-in-anti-gad-associated-encephalomyelitis/. Accessed April 3, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/unilateral-hypertrophic-olivary-degeneration-in-anti-gad-associated-encephalomyelitis/