Category: Parkinson's Disease: Neuroimaging
Objective: We aimed to test the differences of dynamic regional homogeneity (dReHo) between PD patients and healthy controls (HCs), and explore whether dReHo can be utilized to distinguish PD from HCs and further investigate pathophysiological mechanisms of PD.
Background: Only little attention has been paid to the dynamic alterations of regional brain activity in Parkinson disease (PD).
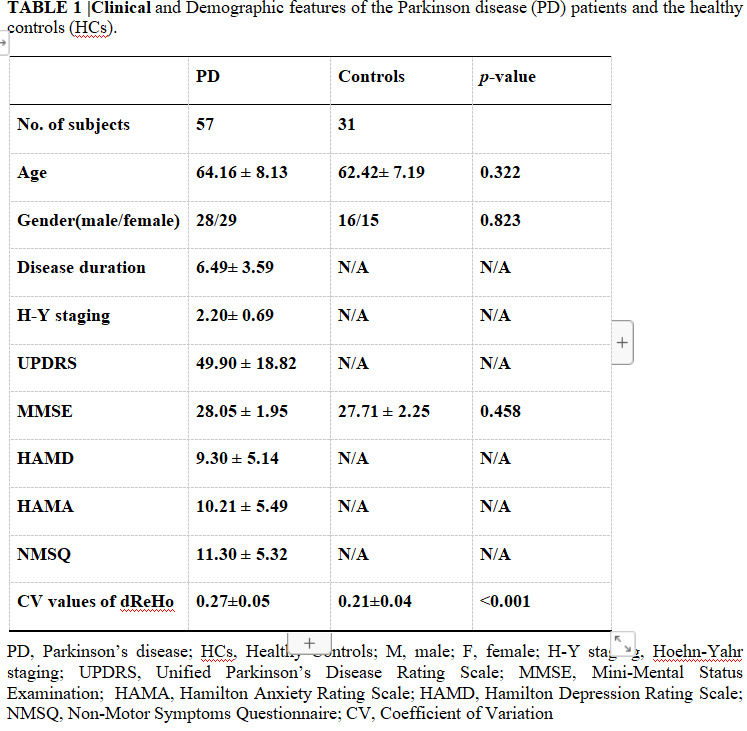
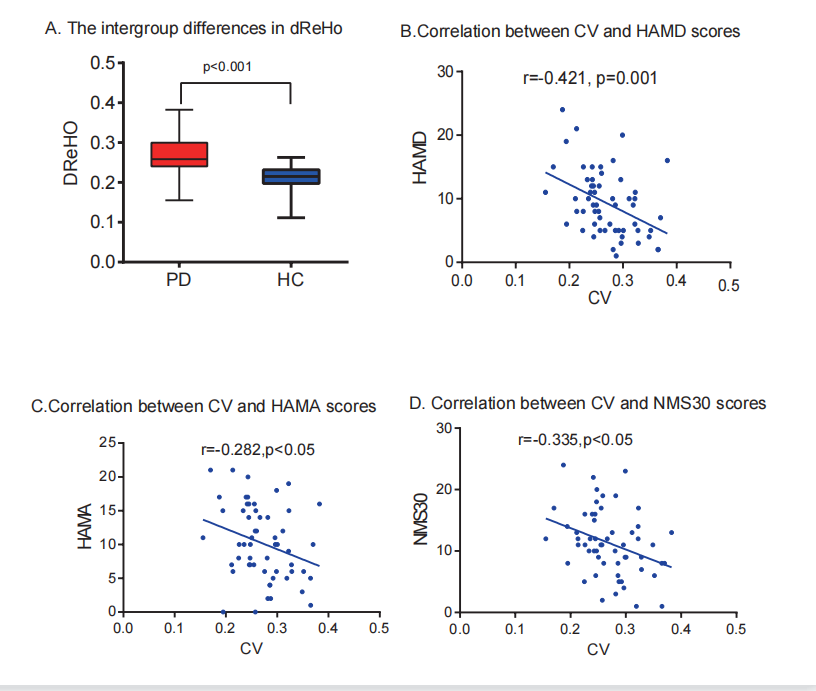
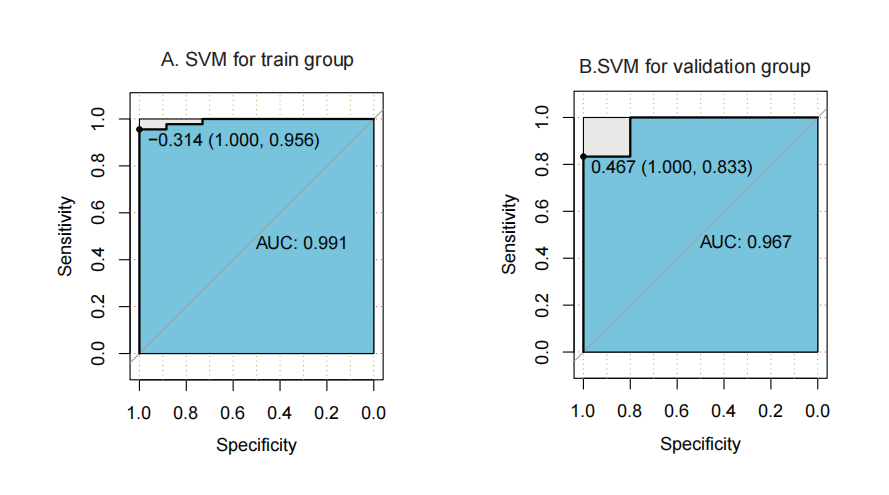
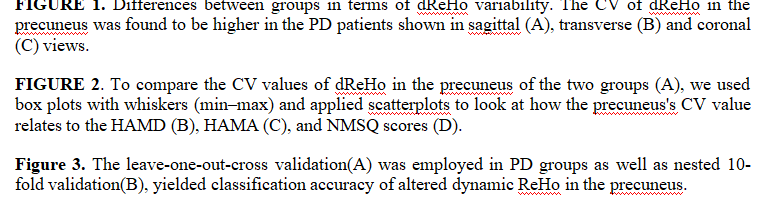
Method: We finally included 57 PD patients and 31 HCs with rs-fMRI scans and neuropsychological examinations. Then dReHo was calculated in all the subjects. We compared dReHo between the PD patients and HCs, then the associations between dReHo variability and clinical/neuropsychological measurements were analyzed. The support vector machines (SVMs) was also used to assist differentiating PD patients from HCs, with the classification values of dReHo.
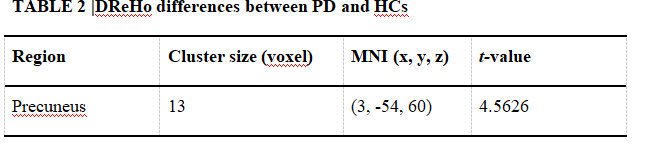
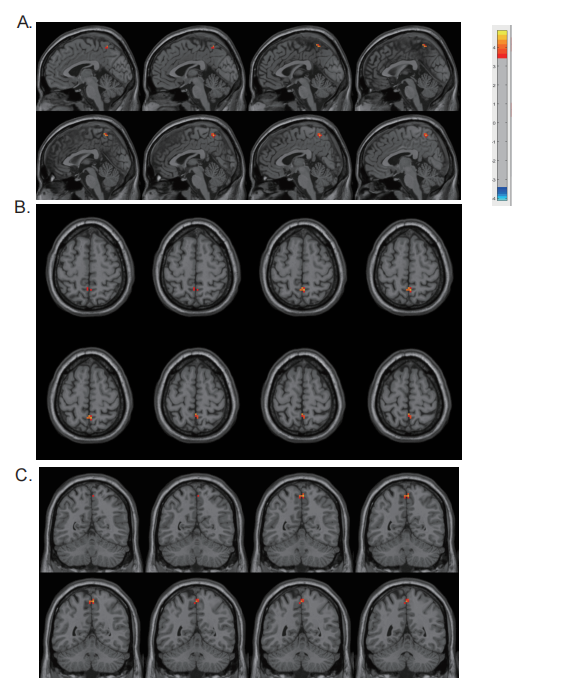
Results: The variation coefficient (CV) of dReHo was increased considerably in the precuneus in PD patients compared with HCs, and the CV of the dReHo in the precuneus was found to be highly associated with HAMD, HAMA, and NMSQ scores. Using the leave-one-out cross-validation procedure, 98 percent (p <0.001) of the individuals were properly identified using the SVM classifier.
Conclusion: These results provide new evidence for the aberrant resting-state brain activity in the precuneus of PD patients, and its role in neuropsychiatric symptoms in PD.
References: Reference
Ashburner, J. (2007). A fast diffeomorphic image registration algorithm. Neuroimage 38, 95–113. doi:10.1016/j.neuroimage.2007.07.007.
Barkhof, F., Haller, S., and Rombouts, S. A. R. B. (2014). Resting-state functional MR imaging: A new window to the brain. Radiology 272, 29–49. doi:10.1148/radiol.14132388.
Borroni, B., Premi, E., Formenti, A., Turrone, R., Alberici, A., Cottini, E., et al. (2015). Structural and functional imaging study in dementia with Lewy bodies and Parkinson’s disease dementia. Park. Relat. Disord. 21, 1049–1055. doi:10.1016/j.parkreldis.2015.06.013.
Cavanna, A. E., and Trimble, M. R. (2006). The precuneus: A review of its functional anatomy and behavioural correlates. Brain 129, 564–583. doi:10.1093/brain/awl004.
Chao-Gan, Y., and Yu-Feng, Z. (2010). DPARSF: A MATLAB toolbox for “pipeline” data analysis of resting-state fMRI. Front. Syst. Neurosci. 4, 1–7. doi:10.3389/fnsys.2010.00013.
Chehebe, J. R. B. (2004). Socialmente responsável. Metal. e Mater. 60, 688–690.
Chen, J., Sun, D., Shi, Y., Jin, W., Wang, Y., Xi, Q., et al. (2019). Dynamic alterations in spontaneous neural activity in multiple brain networks in subacute stroke patients: A resting-state fMRI study. Front. Neurosci. 13. doi:10.3389/fnins.2018.00994.
Chen, X., Zhang, H., Gao, Y., Wee, C. Y., Li, G., and Shen, D. (2016). High-order resting-state functional connectivity network for MCI classification. Hum. Brain Mapp. 37, 3282–3296. doi:10.1002/hbm.23240.
Choe, I. H., Yeo, S., Chung, K. C., Kim, S. H., and Lim, S. (2013). Decreased and increased cerebral regional homogeneity in early Parkinson’s disease. Brain Res. 1527, 230–237. doi:10.1016/j.brainres.2013.06.027.
Emre, M., Aarsland, D., Brown, R., Burn, D. J., Duyckaerts, C., Mizuno, Y., et al. (2007). Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov. Disord. 22, 1689–1707. doi:10.1002/mds.21507.
Friston, K. J., Williams, S., Howard, R., Frackowiak, R. S. J., and Turner, R. (1996). Movement-related effects in fMRI time-series. Magn. Reson. Med. 35, 346–355. doi:10.1002/mrm.1910350312.
Hu, X., Song, X., Li, E., Liu, J., Yuan, Y., Liu, W., et al. (2015). Altered resting-state brain activity and connectivity in depressed Parkinson’s disease. PLoS One 10, 1–13. doi:10.1371/journal.pone.0131133.
Hughes, A. J., Daniel, S. E., Kilford, L., and Lees, A. J. (1992). Accuracy of clinical diagnosis of idiopathic Parkinson ’ s disease : a clinico-pathological study of 100 cases. 181–184.
Jia, X., Li, Y., Li, K., Liang, P., and Fu, X. (2019). Precuneus dysfunction in Parkinson’s disease with mild cognitive impairment. Front. Aging Neurosci. 11, 1–9. doi:10.3389/fnagi.2018.00427.
Jiang, S., Wang, M., Zhang, L., Yuan, Y., Tong, Q., Ding, J., et al. (2016). Regional homogeneity alterations differentiate between tremor dominant and postural instability gait difficulty subtypes of Parkinson’s disease. J. Neural Transm. 123, 219–229. doi:10.1007/s00702-015-1490-5.
Kalia, L. V., and Lang, A. E. (2015). Parkinson’s disease. Lancet 386, 896–912. doi:10.1016/S0140-6736(14)61393-3.
Li, B., Liu, L., Friston, K. J., Shen, H., Wang, L., Zeng, L. L., et al. (2013). A treatment-resistant default mode subnetwork in major depression. Biol. Psychiatry 74, 48–54. doi:10.1016/j.biopsych.2012.11.007.
Liu, F., Guo, W., Yu, D., Gao, Q., Gao, K., Xue, Z., et al. (2012). Classification of different therapeutic responses of major depressive disorder with multivariate pattern analysis method based on structural MR scans. PLoS One 7. doi:10.1371/journal.pone.0040968.
Liu, F., Wang, Y., Li, M., Wang, W., Li, R., Zhang, Z., et al. (2016). Dynamic Functional Network Connectivity in Idiopathic Generalized Epilepsy with Generalized Tonic – Clonic Seizure. 00, 1–17. doi:10.1002/hbm.23430.
Ma, X., Lu, F., Hu, C., Wang, J., Zhang, S., Zhang, S., et al. (2020). Dynamic alterations of spontaneous neural activity in patients with amyotrophic lateral sclerosis.
Manoliu, A., Meng, C., Brandl, F., Doll, A., Tahmasian, M., Scherr, M., et al. (2014). Insular dysfunction within the salience network is associated with severity of symptoms and aberrant inter-network connectivity in major depressive disorder. Front. Hum. Neurosci. 7, 1–17. doi:10.3389/fnhum.2013.00930.
Michel, P. P., Hirsch, E. C., and Hunot, S. (2016). Understanding Dopaminergic Cell Death Pathways in Parkinson Disease. Neuron 90, 675–691. doi:10.1016/j.neuron.2016.03.038.
Miller, D. B., and O’Callaghan, J. P. (2015). Biomarkers of Parkinson’s disease: Present and future. Metabolism. 64, S40–S46. doi:10.1016/j.metabol.2014.10.030.
Nobili, F., Abbruzzese, G., Morbelli, S., Marchese, R., Girtler, N., Dessi, B., et al. (2009). Amnestic mild cognitive impairment in Parkinson’s disease: A brain perfusion SPECT study. Mov. Disord. 24, 414–421. doi:10.1002/mds.22381.
Pan, P., Zhan, H., Xia, M., Zhang, Y., Guan, D., and Xu, Y. (2016). Aberrant regional homogeneity in Parkinson ’ s disease : a voxel -wise meta-analysis of resting-state functional magnetic resonance imaging. Elsevier Ltd doi:10.1016/j.neubiorev.2016.11.018.
Shin, J. H., Shin, S. A., Lee, J. Y., Nam, H., Lim, J. S., and Kim, Y. K. (2017). Precuneus degeneration and isolated apathy in patients with Parkinson’s disease. Neurosci. Lett. 653, 250–257. doi:10.1016/j.neulet.2017.05.061.
Sveinbjornsdottir, S. (2016). The clinical symptoms of Parkinson’s disease. J. Neurochem., 318–324. doi:10.1111/jnc.13691.
Syrimi, Z. J., Vojtisek, L., Eliasova, I., Viskova, J., Svatkova, A., Vanicek, J., et al. (2017). Arterial spin labelling detects posterior cortical hypoperfusion in non-demented patients with Parkinson’s disease. J. Neural Transm. 124, 551–557. doi:10.1007/s00702-017-1703-1.
Tang, C. C., Poston, K. L., Dhawan, V., and Eidelberg, D. (2010). Abnormalities in metabolic network activity precede the onset of motor symptoms in Parkinson’s disease. J. Neurosci. 30, 1049–1056. doi:10.1523/JNEUROSCI.4188-09.2010.
Tang, C., Wei, Y., Zhao, J., and Nie, J. (2018). The dynamic measurements of regional brain activity for resting-state fMRI: d-ALFF, d-fALFF and d-ReHo. in International Conference on Medical Image Computing and Computer-Assisted Intervention (Springer), 190–197.
Thibes, R. B., Novaes, N. P., Lucato, L. T., Campanholo, K. R., Melo, L. M., Leite, C. C., et al. (2017). Altered Functional Connectivity between Precuneus and Motor Systems in Parkinson’s Disease Patients. Brain Connect. 7, 643–647. doi:10.1089/brain.2017.0534.
Wang, J., Zhang, J., and Zang, Y. (2018). Consistent decreased activity in the putamen in Parkinson ’ s disease : a meta-analysis and an independent validation of resting-state fMRI. 1–13. doi:10.1093/gigascience/giy071.
Wee, C. Y., Yang, S., Yap, P. T., and Shen, D. (2016). Sparse temporally dynamic resting-state functional connectivity networks for early MCI identification. Brain Imaging Behav. 10, 342–356. doi:10.1007/s11682-015-9408-2.
Yan, C. G., Yang, Z., Colcombe, S. J., Zuo, X. N., and Milham, M. P. (2017). Concordance among indices of intrinsic brain function: Insights from inter-individual variation and temporal dynamics. Science China Press doi:10.1016/j.scib.2017.09.015.
Yan, C., Wang, X., Zuo, X., and Zang, Y. (2016). DPABI : Data Processing & Analysis for ( Resting-State ) Brain Imaging. Neuroinformatics. doi:10.1007/s12021-016-9299-4.
Yan, J., Li, M., Fu, S., Li, G., Wang, T., and Yin, Y. (2019). Alterations of Dynamic Regional Homogeneity in Trigeminal Neuralgia : A Resting-State fMRI Study. 10, 1–6. doi:10.3389/fneur.2019.01083.
Yu, Y., Li, Z., Lin, Y., Yu, J., Peng, G., Zhang, K., et al. (2019). Depression Affects Intrinsic Brain Activity in Patients With Mild Cognitive Impairment. 13, 1–9. doi:10.3389/fnins.2019.01333.
Zalesky, A., and Breakspear, M. (2015). NeuroImage Towards a statistical test for functional connectivity dynamics. Neuroimage. doi:10.1016/j.neuroimage.2015.03.047.
Zang, Y., Jiang, T., Lu, Y., He, Y., and Tian, L. (2004). Regional homogeneity approach to fMRI data analysis. Neuroimage 22, 394–400. doi:10.1016/j.neuroimage.2003.12.030.
Zanigni, S., Sambati, L., Evangelisti, S., Testa, C., Calandra-Buonaura, G., Manners, D. N., et al. (2017). Precuneal Thickness and Depression in Parkinson Disease. Neurodegener. Dis. 17, 97–102. doi:10.1159/000450614.
Zhang, C., Dou, B., Wang, J., Xu, K., Zhang, H., Sami, M. U., et al. (2019a). Dynamic Alterations of Spontaneous Neural Activity in Parkinson’s Disease: A Resting-State fMRI Study. Front. Neurol. 10. doi:10.3389/fneur.2019.01052.
To cite this abstract in AMA style:
T. Yuan, L. Kai, S. Wen. Temporal Dynamic Alterations of Regional Homogeneity in Parkinson’s disease: A Resting-State fMRI Study [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/temporal-dynamic-alterations-of-regional-homogeneity-in-parkinsons-disease-a-resting-state-fmri-study/. Accessed December 17, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/temporal-dynamic-alterations-of-regional-homogeneity-in-parkinsons-disease-a-resting-state-fmri-study/