Category: Rare Genetic and Metabolic Diseases
Objective: To describe the clinical, imaging and genetic profile of patients with suspected NBIA disorders
Background: NBIA disorders are clinically, radiologically and genetically heterogenous group affecting all age groups worldwide. Although iron deposition was thought to be the common pathology, various other biochemical pathways in cell can be affected leading to free radicle damage and secondary iron deposition ranging from significant to no deposition at all. It is important to understand this wide spectrum of heterogeneity for future research and management.
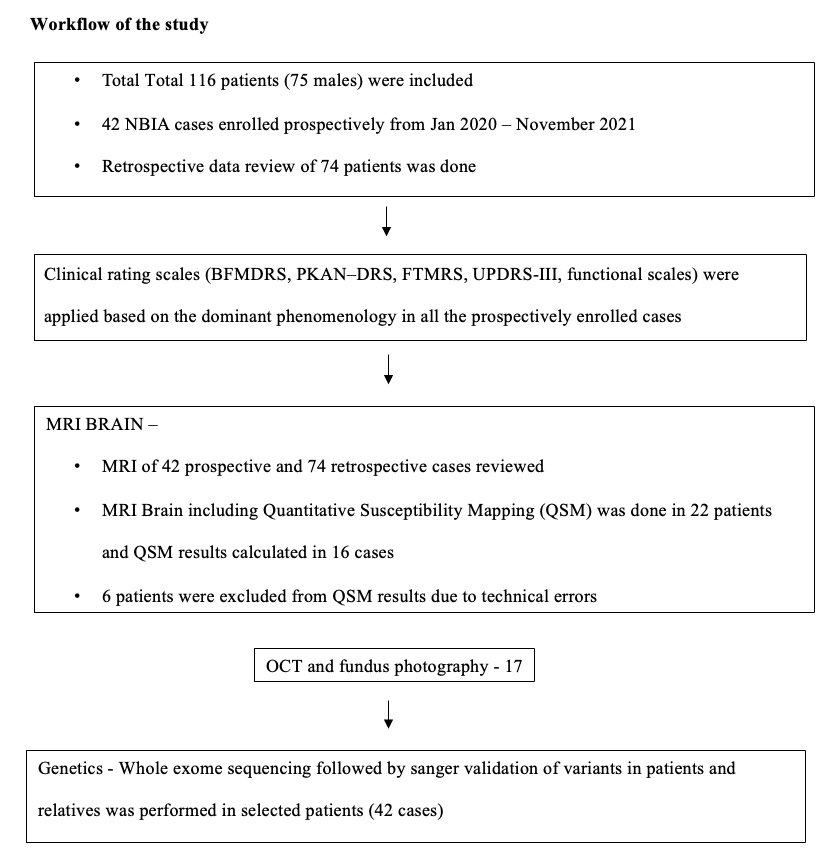
Method: An ambispective hospital-based single centre study conducted at department of Neurology of a tertiary care centre [Table1]. Demographic, neurological and ophthalmological details were tabulated. Clinical rating scales were applied in all the prospectively enrolled cases. MRI Brain including Quantitative Susceptibility Mapping (QSM) and whole exome sequencing followed by sanger validation of variants in patients and relatives was performed in selected patients.
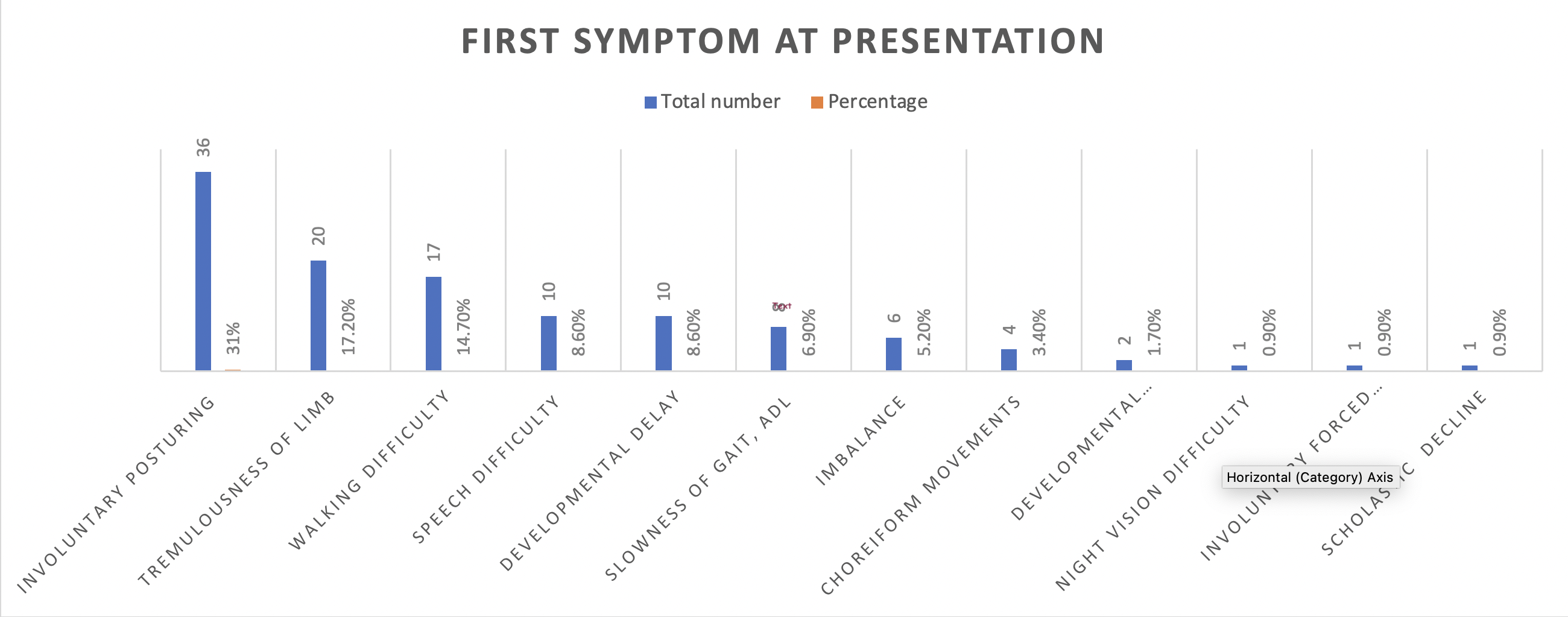
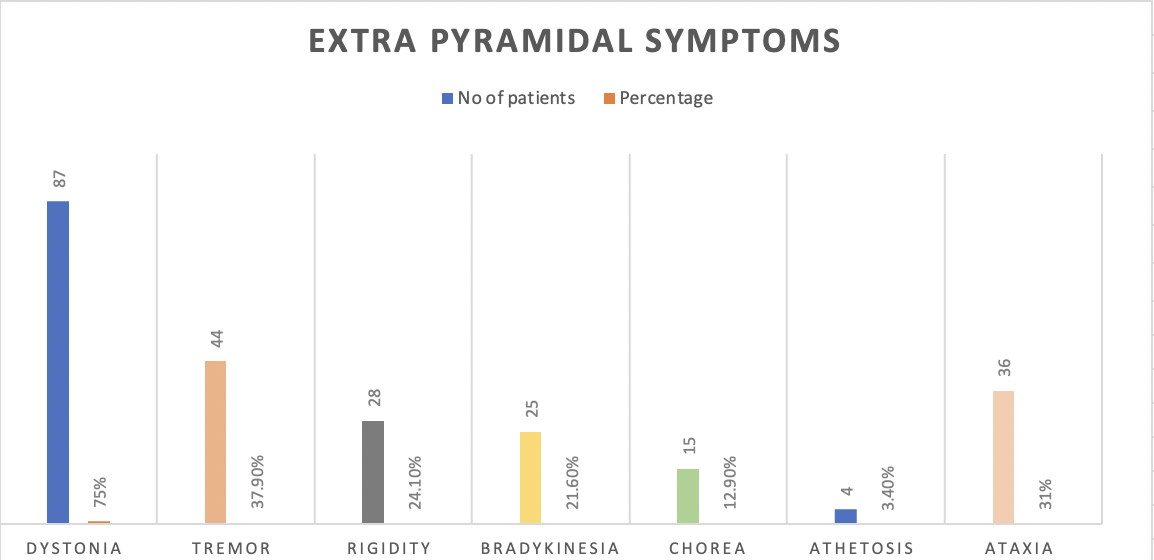
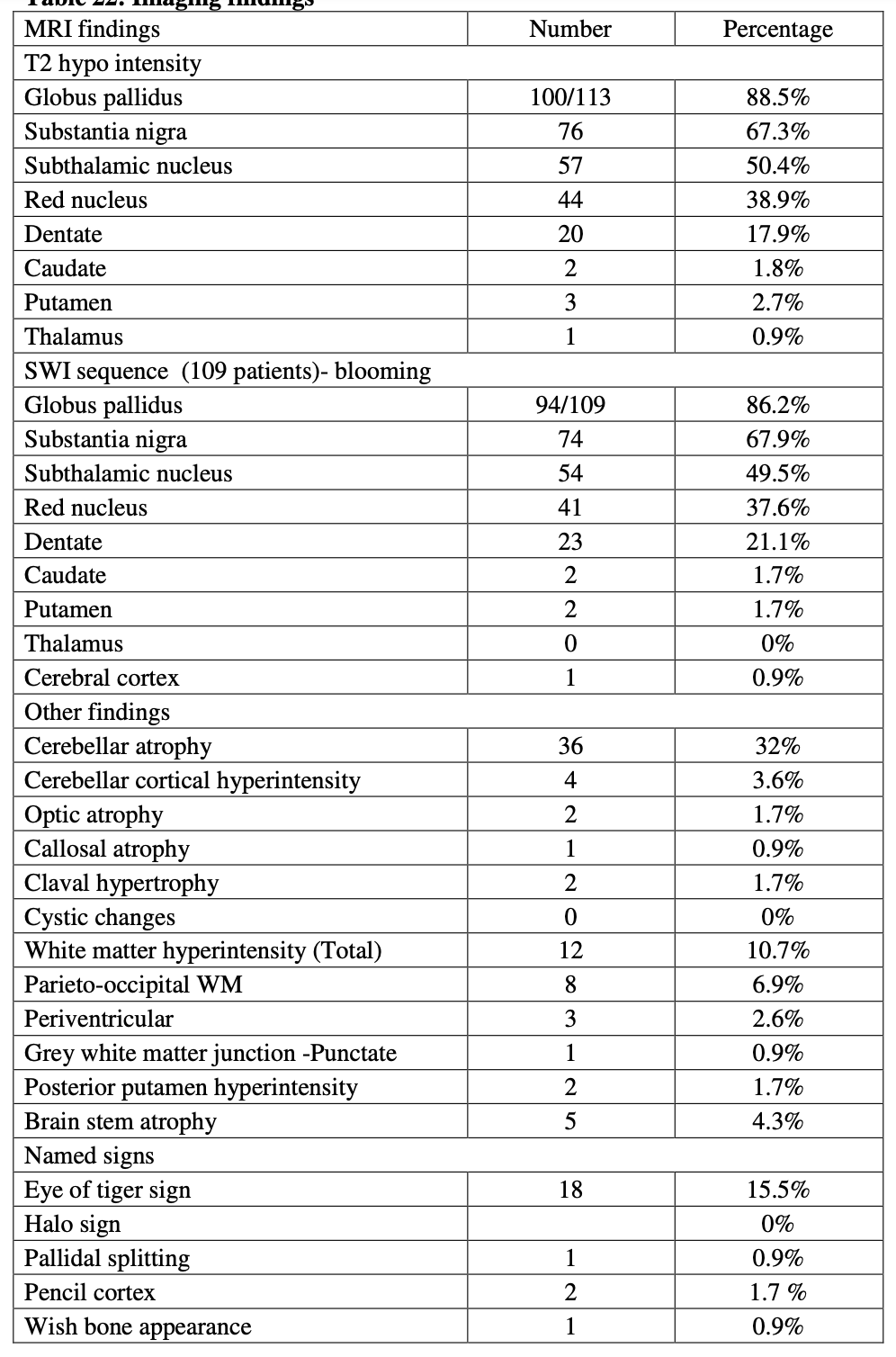
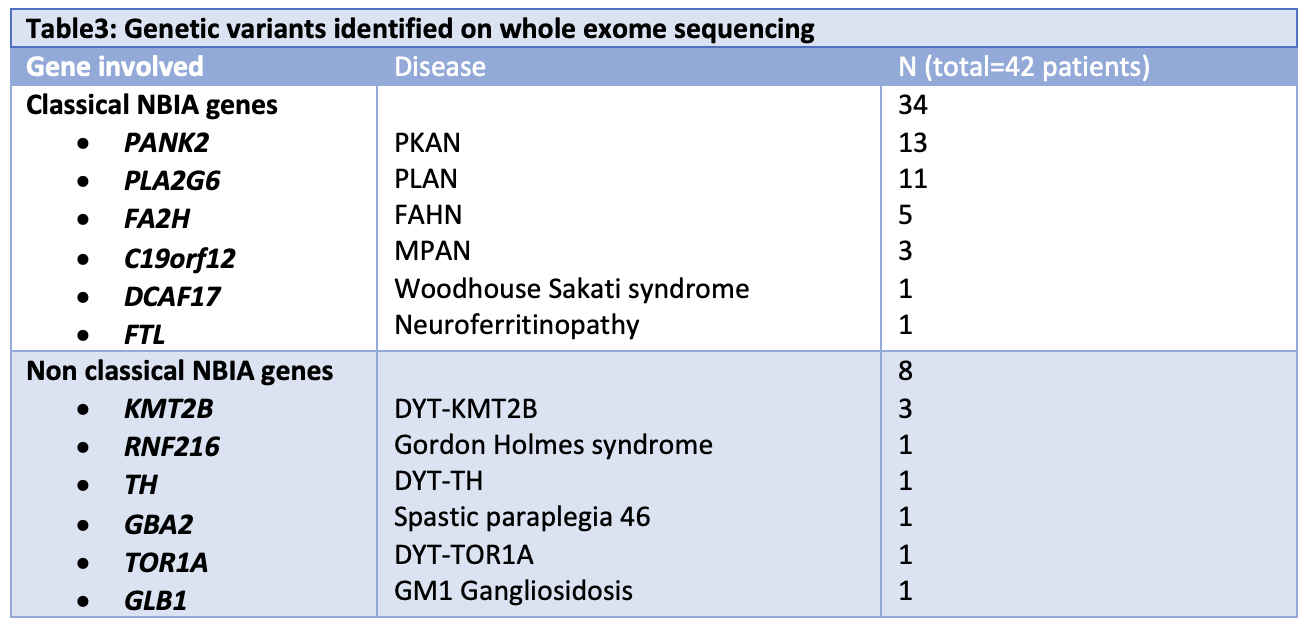
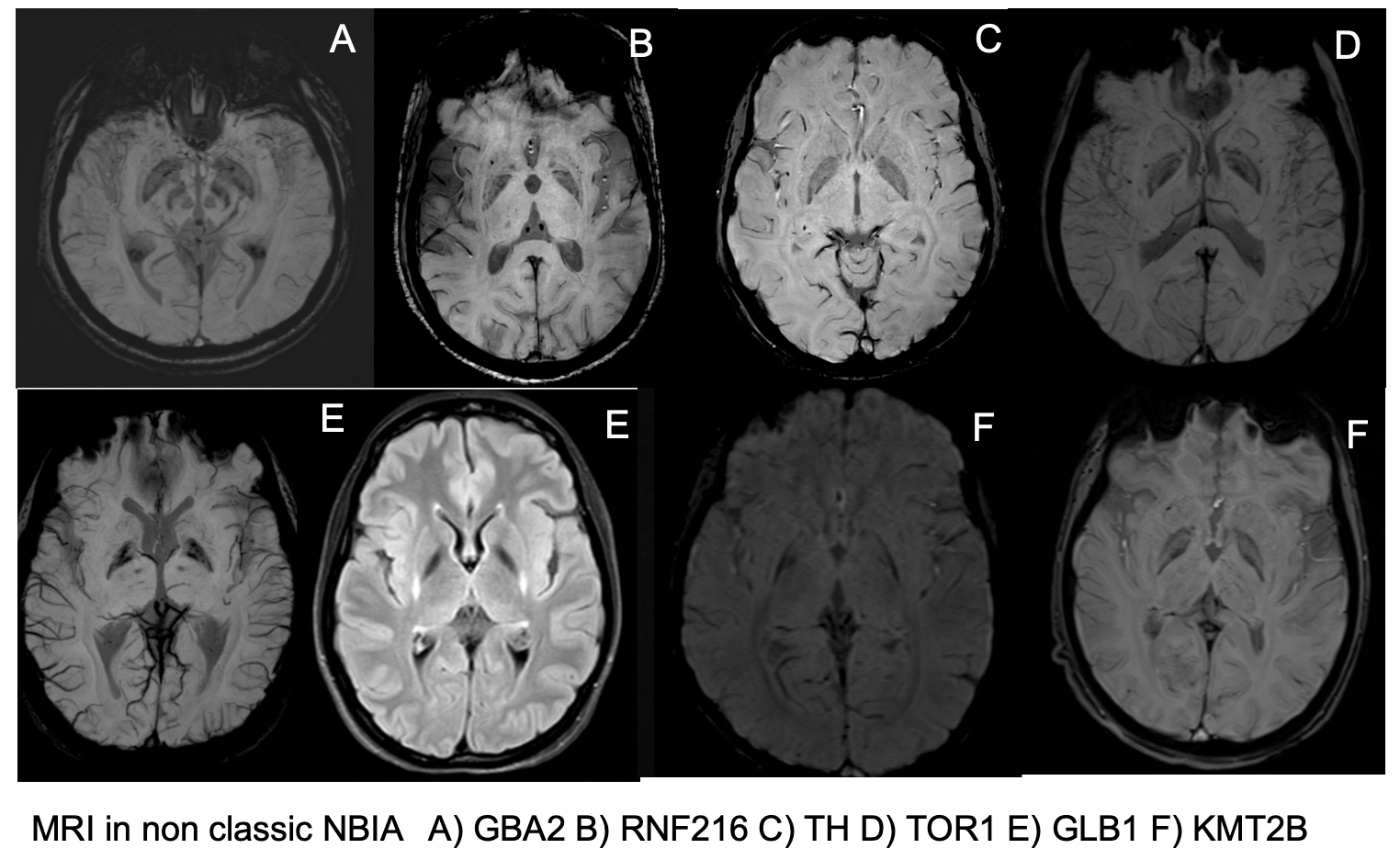
Results: Total 116 patients (75 males) were included with median age at onset and at presentation of 12y (Range: 0-50y) and 22y (Range: 0.7-65y) respectively. 56% had onset before the age of 10 years. Dystonia was both the commonest symptom at onset (31%) [Figure1] and the most common extrapyramidal phenomenology (75%) [Figure2]. On MRI Brain SWI sequence, mineralization was most frequent in globus pallidus (86.2%) [Table2]. Eye of tiger sign was present in 15.5% (81.8% of suspected PKAN), whereas pallidal splitting, pencil cortex and wish bone appearance were found in 0.9% each. Retinitis pigmentosa was seen in 6/22 (27%) PKAN patients. OCT showed thinning of RNFL in 3/16 patients. QSM scores (available for 16 patients) of GP correlated inversely with FMDRS and PKAN-DRS while there was no correlation between rating scores and QSM scores of putamen, caudate, SN, RN, dentate. Among 42 patients who underwent WES, 34 had pathogenic/likely pathogenic variants in classical NBIA genes and 8 had variants in non-classical NBIA genes [Table3, Figure 3].
Conclusion: Mineralisation was absent on MRI in 14% cases in our study. Absence of correlation between clinical severity and QSM scores in 16 patients suggest mineralisation could be a secondary phenomenon. PANK2 and PLA2G6 were the most common gene involved and around 1/6th of the cohort had abnormalities in genes not classically associated with NBIA.
To cite this abstract in AMA style:
N. Sriram, P. Pal, V. Holla, N. Kamble, J. Saini, R. Yadav, RAJ. Battu, VY. K N, B. Muthusamy, RI. Kumari. Clinical, imaging and genetic profile of patients with NBIA spectrum disorders [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/clinical-imaging-and-genetic-profile-of-patients-with-nbia-spectrum-disorders/. Accessed February 6, 2026.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/clinical-imaging-and-genetic-profile-of-patients-with-nbia-spectrum-disorders/