Category: Technology
Objective: To develop an easily accessible and objective tool to evaluate gait in PD patients, we analyzed gait from a single 2-dimensional (2D) video.
Background: Clinician based rating scales or questionnaires for gait in Parkinson’s disease (PD) are subjective and sensor-based analysis is limited in accessibility
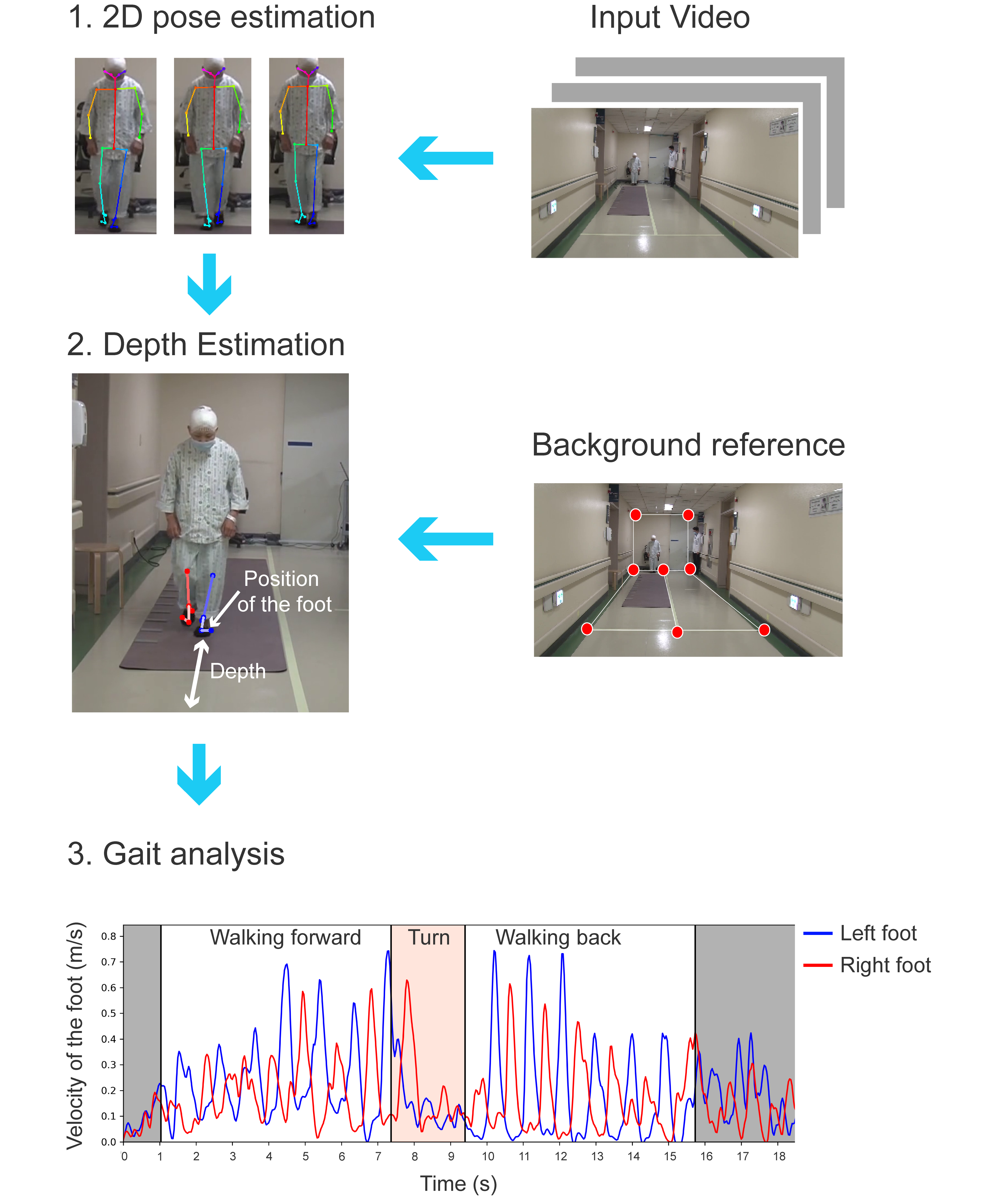
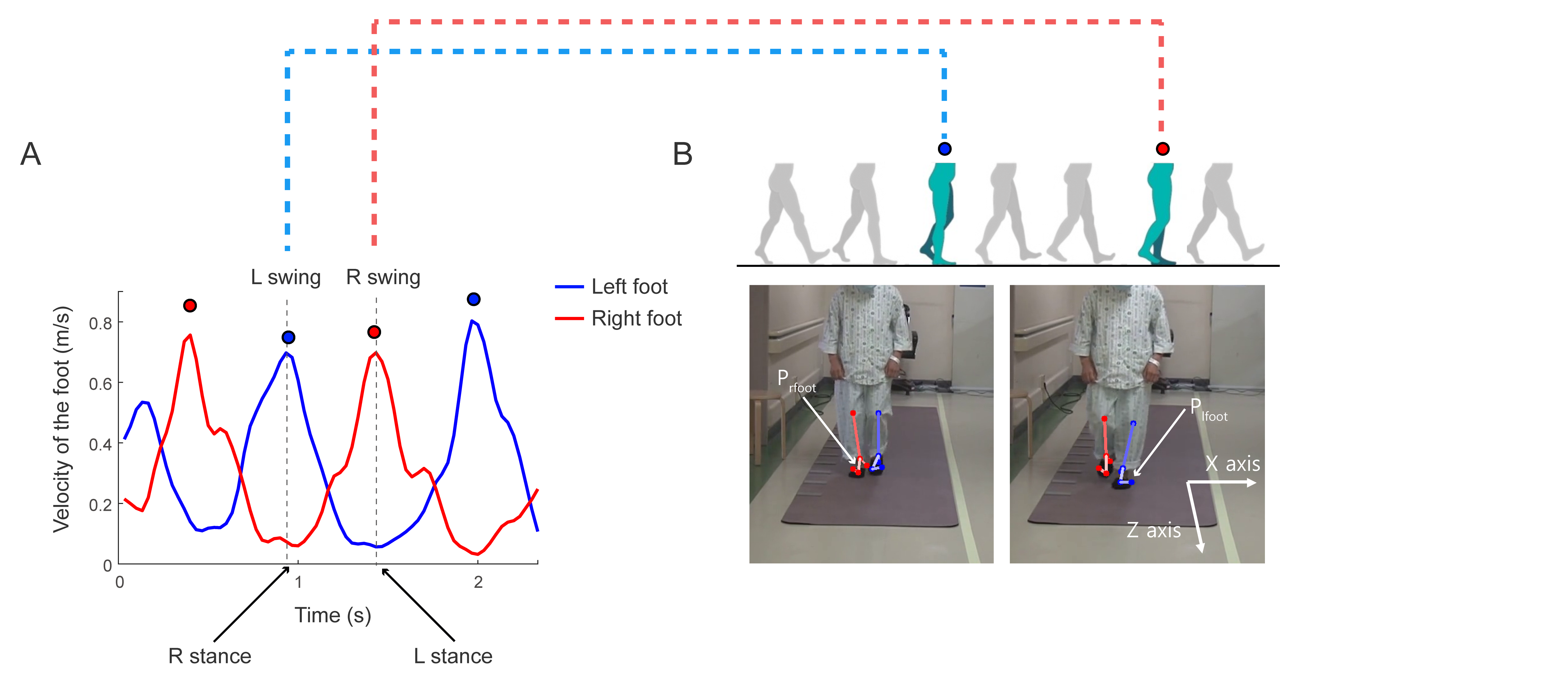
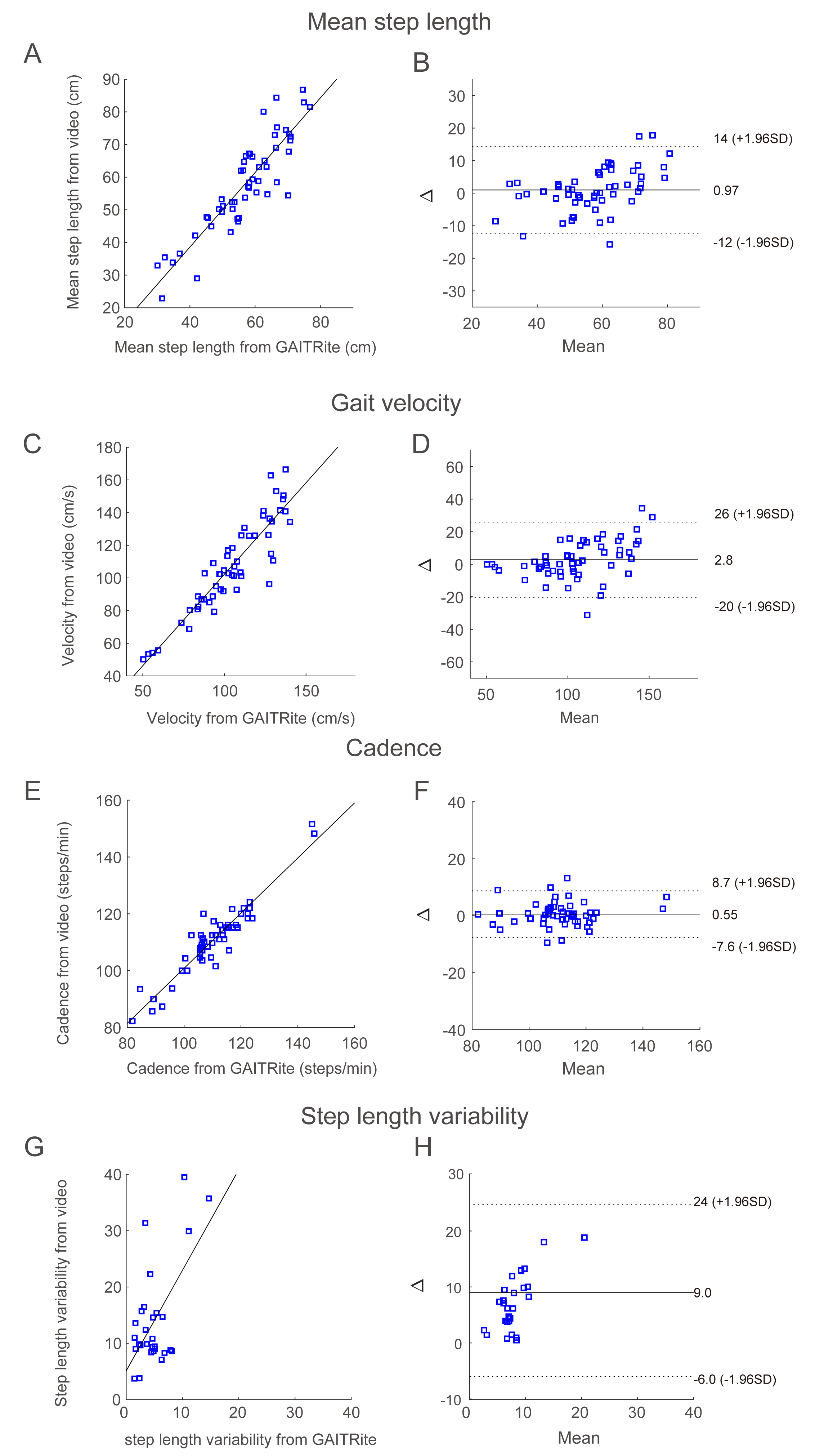
Method: We prospectively recorded 2D videos of PD patients (n=16) and healthy controls (n=15) performing the timed up and go test (TUG). The gait was simultaneously evaluated with a pressure-sensor (GAITRite). We estimated 3D position of toes and heels with a deep-learning based pose-estimation algorithm and calculated gait parameters including step length, step length variability, gait velocity and step cadence which was validated with the result from the GAITRite. We further calculated the time and steps required for turning. Steps required for turning was validated with manual measure. Then, we applied the algorithm to archieved videos of PD patients (n=32) performing the TUG
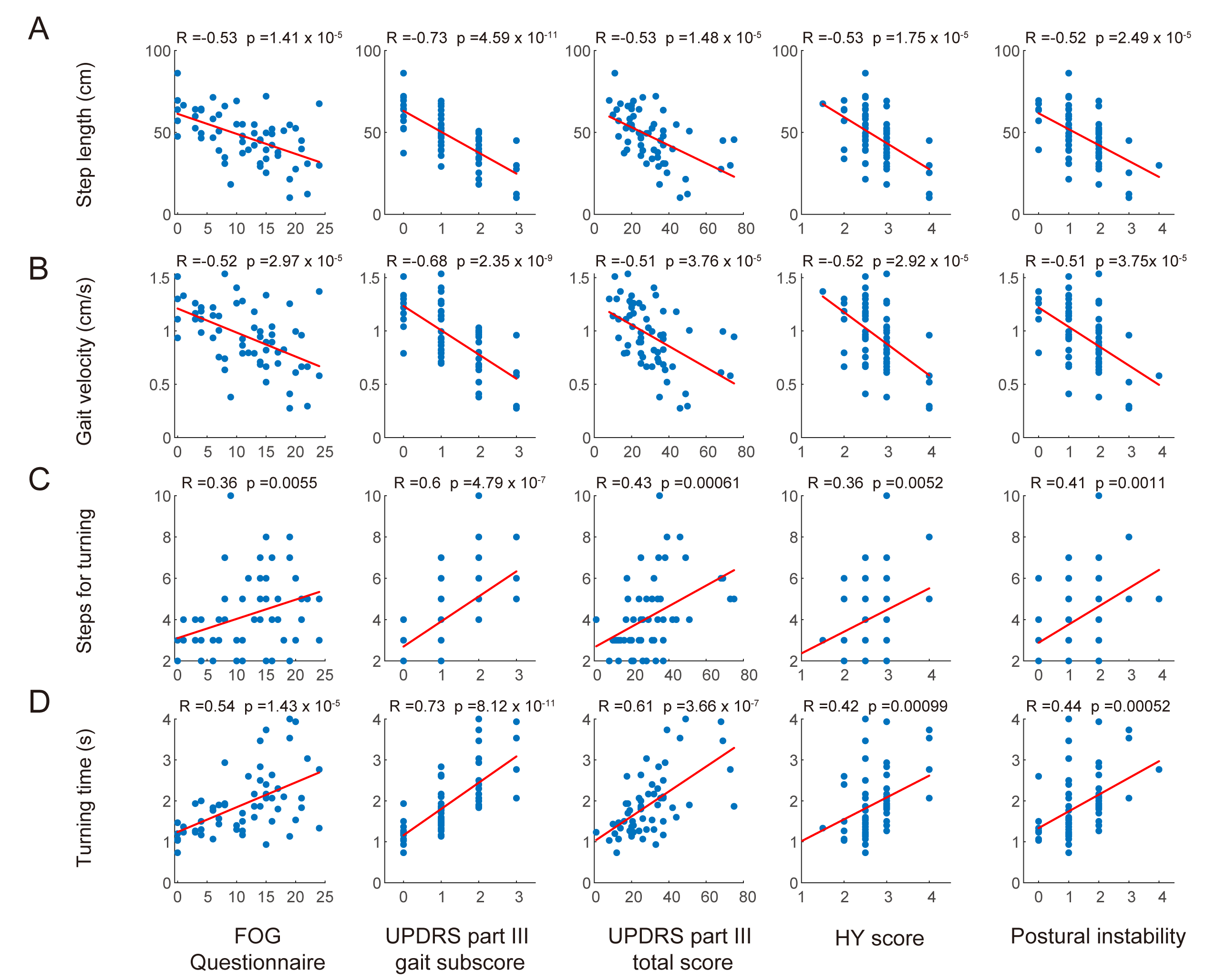
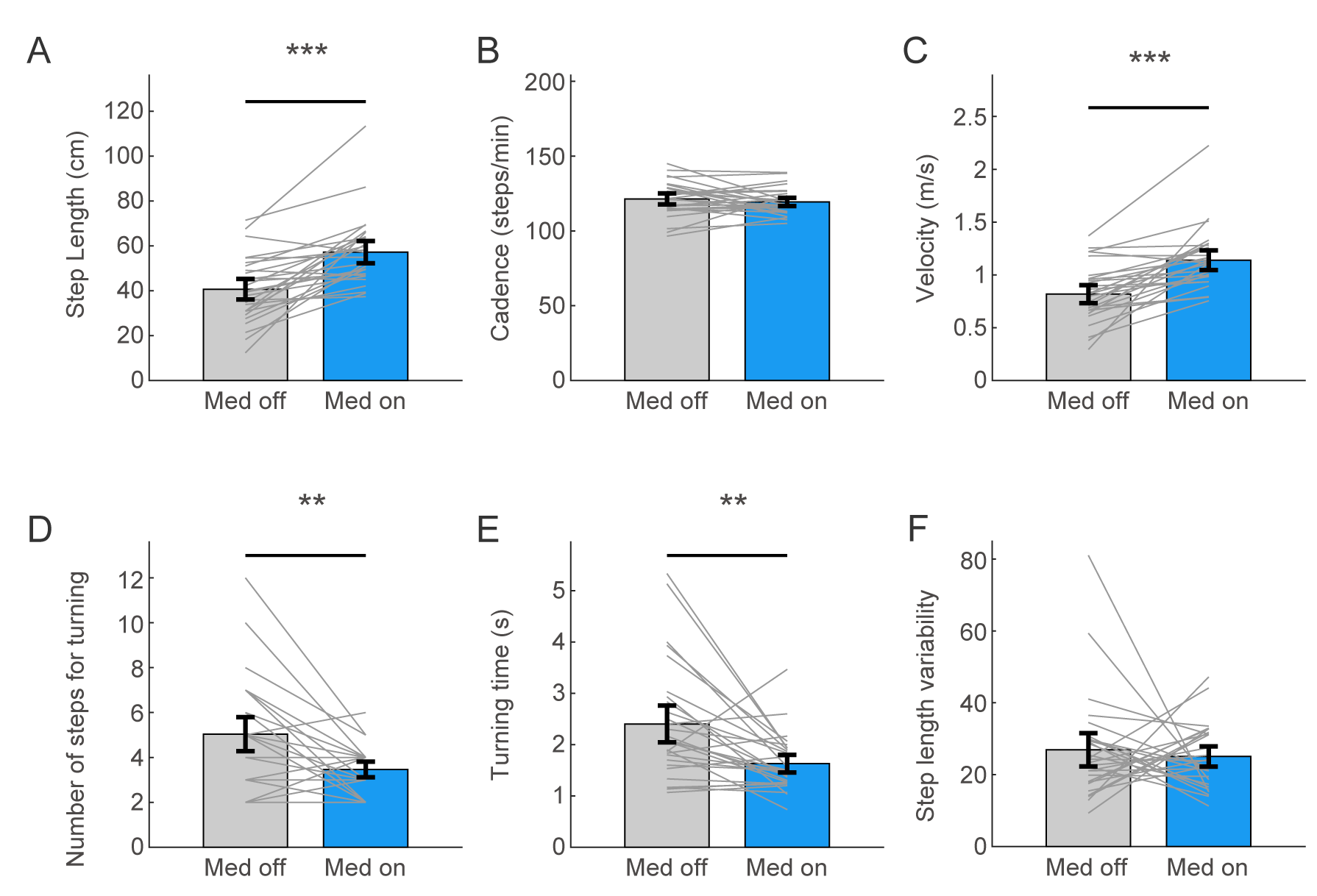
Results: From the validation experiment, gait parameters derived from video tracking were in excellent agreement with the parameters obtained with the GAITRite. (Intraclass correlation coefficient > 0.9). From the analysis with the archieved videos, Step length, gait velocity, number of steps and the time required for turning were significantly correlated (Absolute R > 0.4, p < 0.005) with the Freezing of gait questionnaire, Unified PD Rating scale part III total score, HY stage and postural instability. Furthermore, the video-based tracking objectively measured significant improvement of step length, gait velocity, steps and the time required for turning with antiparkinsonian medication.
Conclusion: The video-based gait analysis can reliably and objectively measure gait parameters with 2D videos of PD patients. This study quantitatively analyzed the gait of PD patients with a “marker-less” and “automated” algorithm using 2D video. Quantitative gait analysis using accessible and cost-effective 2D videos has the potential to be widely used in daily practice as an objective measurement in research and clinical practice.
References: [1] Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30, 1591-1601. [2] Vervoort G, Bengevoord A, Strouwen C, Bekkers EM, Heremans E, Vandenberghe W, Nieuwboer A (2016) Progression of postural control and gait deficits in Parkinson’s disease and freezing of gait: A longitudinal study. Parkinsonism Relat Disord 28, 73-79. [3] Morris ME, Iansek R, Matyas TA, Summers JJ (1994) The pathogenesis of gait hypokinesia in Parkinson’s disease. Brain 117 ( Pt 5), 1169-1181. [4] Walton CC, Shine JM, Hall JM, O’Callaghan C, Mowszowski L, Gilat M, Szeto JY, Naismith SL, Lewis SJ (2015) The major impact of freezing of gait on quality of life in Parkinson’s disease. J Neurol 262, 108-115. [5] Bloem BR, Hausdorff JM, Visser JE, Giladi N (2004) Falls and freezing of gait in Parkinson’s disease: a review of two interconnected, episodic phenomena. Mov Disord 19, 871-884. [6] Fahn S (1987) Unified Parkinson’s disease rating scale. Recent developments in Parkinson’s disease volume II. Macmillan Healthcare Information 153. [7] Ramaker C, Marinus J, Stiggelbout AM, Van Hilten BJ (2002) Systematic evaluation of rating scales for impairment and disability in Parkinson’s disease. Mov Disord 17, 867-876. [8] Richards M, Marder K, Cote L, Mayeux R (1994) Interrater reliability of the Unified Parkinson’s Disease Rating Scale motor examination. Mov Disord 9, 89-91. [9] Post B, Merkus MP, de Bie RM, de Haan RJ, Speelman JD (2005) Unified Parkinson’s disease rating scale motor examination: are ratings of nurses, residents in neurology, and movement disorders specialists interchangeable? Mov Disord 20, 1577-1584. [10] Giladi N, Shabtai H, Simon ES, Biran S, Tal J, Korczyn AD (2000) Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord 6, 165-170. [11] Tinetti ME, Williams TF, Mayewski R (1986) Fall risk index for elderly patients based on number of chronic disabilities. Am J Med 80, 429-434. [12] Nieuwboer A, Rochester L, Herman T, Vandenberghe W, Emil GE, Thomaes T, Giladi N (2009) Reliability of the new freezing of gait questionnaire: agreement between patients with Parkinson’s disease and their carers. Gait Posture 30, 459-463. [13] Mancini M, Horak FB (2010) The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Rehabil Med 46, 239-248. [14] Muro-de-la-Herran A, Garcia-Zapirain B, Mendez-Zorrilla A (2014) Gait analysis methods: an overview of wearable and non-wearable systems, highlighting clinical applications. Sensors (Basel) 14, 3362-3394. [15] de Oliveira Gondim ITG, de Souza CCB, Rodrigues MAB, Azevedo IM, de Sales Coriolano M, Lins OG (2020) Portable accelerometers for the evaluation of spatio-temporal gait parameters in people with Parkinson’s disease: an integrative review. Arch Gerontol Geriatr 90, 104097. [16] Sofuwa O, Nieuwboer A, Desloovere K, Willems AM, Chavret F, Jonkers I (2005) Quantitative gait analysis in Parkinson’s disease: comparison with a healthy control group. Arch Phys Med Rehabil 86, 1007-1013. [17] Del Din S, Elshehabi M, Galna B, Hobert MA, Warmerdam E, Suenkel U, Brockmann K, Metzger F, Hansen C, Berg D, Rochester L, Maetzler W (2019) Gait analysis with wearables predicts conversion to parkinson disease. Ann Neurol 86, 357-367. [18] Bhidayasiri R, Tarsy D (2012) Movement disorders: a video atlas, Springer Science & Business Media. [19] Shin JH, Ong JN, Kim R, Park S-m, Choi J, Kim H-J, Jeon BJP, Disorders R (2020) Objective measurement of limb bradykinesia using a marker-less tracking algorithm with 2D-video in PD patients. [20] Sahak (2019) Review on Current Methods of Gait Analysis and Recognition using Kinect. IEEE. [21] Michelini A, Eshraghi A, Andrysek J (2020) Two-dimensional video gait analysis: A systematic review of reliability, validity, and best practice considerations. Prosthet Orthot Int, 309364620921290. [22] Kidziński Ł, Yang B, Hicks JL, Rajagopal A, Delp SL, Schwartz MH (2020) Deep neural networks enable quantitative movement analysis using single-camera videos. Nature Communications 11, 4054. [23] Cho C-W, Chao W-H, Lin S-H, Chen Y-Y (2009) A vision-based analysis system for gait recognition in patients with Parkinson’s disease. Expert Systems with Applications 36, 7033-7039. [24] Yu H, Kang K, Jeong S, Park J (2019) Deep Vision System for Clinical Gait Analysis in and Out of Hospital In Neural Information Processing, pp. 633-642. [25] Stricker M, Hinde D, Rolland A, Salzman N, Watson A, Almonroeder TG (2019) Quantifying step length using two-dimensional video in individuals with Parkinson’s disease. Physiother Theory Pract, 1-4. [26] Sato K, Nagashima Y, Mano T, Iwata A, Toda T (2019) Quantifying normal and parkinsonian gait features from home movies: Practical application of a deep learning-based 2D pose estimator. PLoS One 14, e0223549. [27] Cao Z, Hidalgo G, Simon T, Wei S-E, Sheikh YJae-p (2018), p. arXiv:1812.08008. [28] Kanazawa A, Zhang JY, Felsen P, Malik JJae-p (2018), p. arXiv:1812.01601. [29] Pavllo D, Feichtenhofer C, Grangier D, Auli MJae-p (2018), p. arXiv:1811.11742. [30] Kocabas M, Athanasiou N, Black MJJae-p (2019), p. arXiv:1912.05656. [31] Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55, 181-184. [32] Koo TK, Li MY (2016) A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med 15, 155-163. [33] Herman T, Giladi N, Hausdorff JM (2011) Properties of the ‘timed up and go’ test: more than meets the eye. Gerontology 57, 203-210. [34] McNeely ME, Earhart GM (2011) The effects of medication on turning in people with Parkinson disease with and without freezing of gait. J Parkinsons Dis 1, 259-270. [35] Youn J, Okuma Y, Hwang M, Kim D, Cho JW (2017) Falling Direction can Predict the Mechanism of Recurrent Falls in Advanced Parkinson’s Disease. Scientific Reports 7, 3921. [36] Hong M, Perlmutter JS, Earhart GM (2009) A kinematic and electromyographic analysis of turning in people with Parkinson disease. Neurorehabil Neural Repair 23, 166-176. [37] Miller Koop M, Ozinga SJ, Rosenfeldt AB, Alberts JL (2018) Quantifying turning behavior and gait in Parkinson’s disease using mobile technology. IBRO Rep 5, 10-16. [38] Rochester L, Baker K, Nieuwboer A, Burn D (2011) Targeting dopa-sensitive and dopa-resistant gait dysfunction in Parkinson’s disease: selective responses to internal and external cues. Mov Disord 26, 430-435. [39] Curtze C, Nutt JG, Carlson-Kuhta P, Mancini M, Horak FB (2015) Levodopa Is a Double-Edged Sword for Balance and Gait in People With Parkinson’s Disease. Mov Disord 30, 1361-1370. [40] Smulders K, Dale ML, Carlson-Kuhta P, Nutt JG, Horak FB (2016) Pharmacological treatment in Parkinson’s disease: Effects on gait. Parkinsonism Relat Disord 31, 3-13.
To cite this abstract in AMA style:
JH. Shin, R. Yu, JN. Ong, CY. Lee, SH. Jeon, HP. Park, HJ. Kim, JH. Lee, B. Jeon. Quantitative gait analysis using a pose-estimation algorithm with a single 2D-video of PD patients [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/quantitative-gait-analysis-using-a-pose-estimation-algorithm-with-a-single-2d-video-of-pd-patients/. Accessed January 2, 2026.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/quantitative-gait-analysis-using-a-pose-estimation-algorithm-with-a-single-2d-video-of-pd-patients/