Category: Surgical Therapy: Parkinson's Disease
Objective: To report on the prevalence of and motivation for directional DBS programming in PD and ET over time.
Background: Directional deep brain stimulation (d-DBS) axially displaces the VTA towards the intended target and away from neighboring structures potentially improving benefit and reducing side effects (SE) of stimulation. A large clinical trial evaluating d-DBS has demonstrated a wider therapeutic window (TW) with directional electrodes.1 While a large TW intuitively seems advantageous, it is not clear how often and for what reason directional stimulation is used in clinical practice, especially in light of time constraints. To evaluate the implementation of d-DBS systems in our center we sought to evaluate the prevalence of and motivation for programming with directional electrodes.
Method: A retrospective chart review was completed in PD and ET patients that were implanted with the Abbott Infinity Directional DBS system from Oct 2016 to Jan 2020. At 3, 12, 24, and 36 months, post-operatively the following information was collected: stimulation parameters including use of directional stimulation and other advanced programming techniques; and reason for use of directional stimulation.
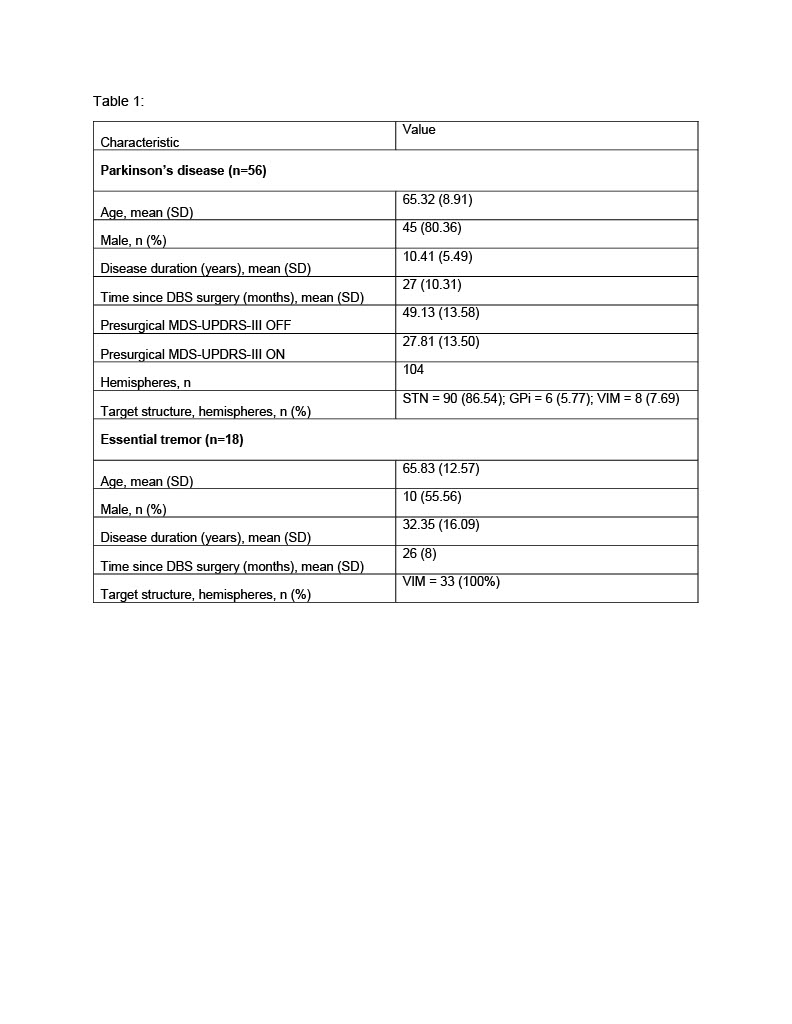
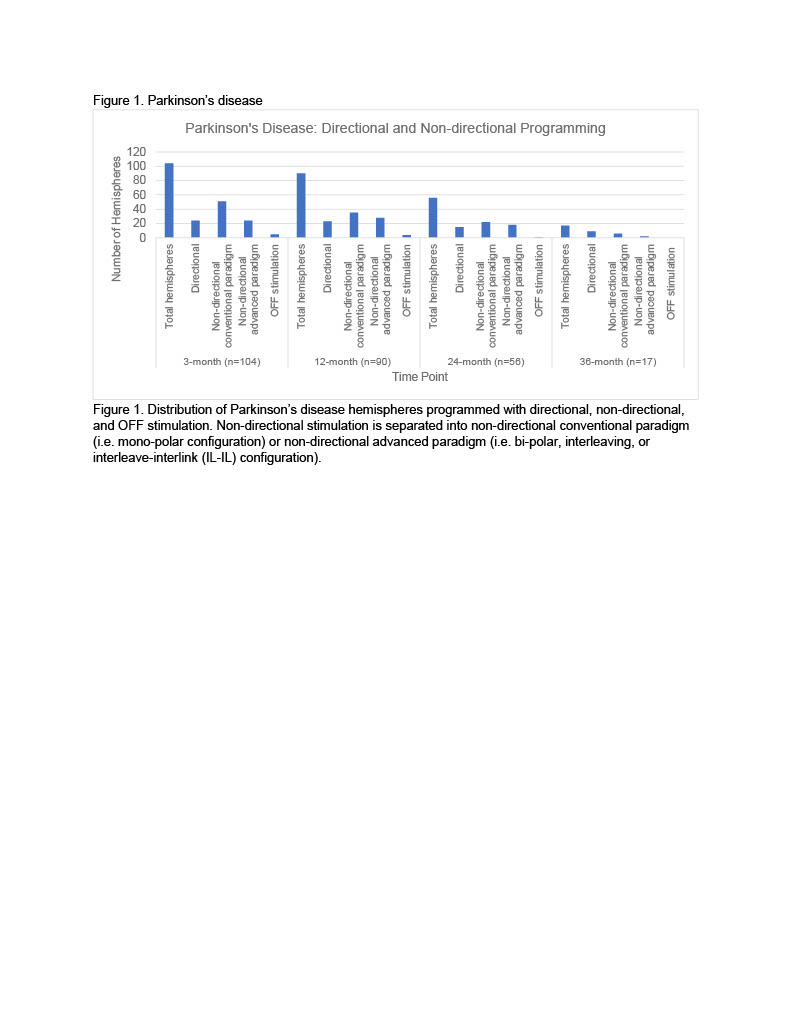
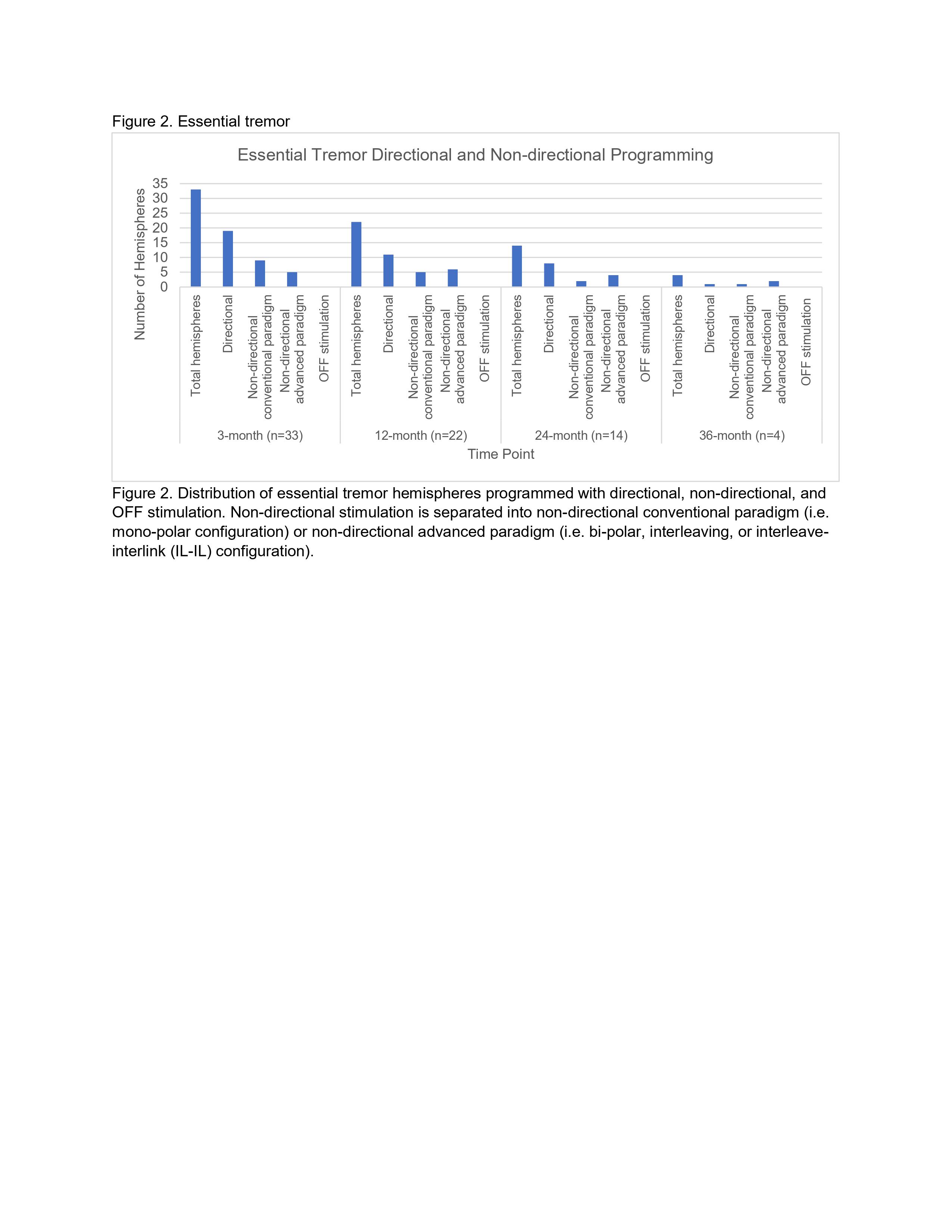
Results: Fifty-six PD and 18 ET patients (104 and 33 hemispheres, respectively) were identified [table 1]. The number of hemispheres programmed with directional stimulation in PD and ET patients, respectively, were 24 (23%) and 19 (58%) at 3 months; 23 (26%) and 11 (50%) at 12 months; 15 (27%) and 8 (57%) at 24-months, and 9 (53%) and 1 (25%) at 36-months [figures1,2]. In PD, reasons for using directional stimulation were better symptom control (75%), reduced SE (22%), or combination of symptom control/SE (3%); in ET, improved battery use/TW% (35%), better symptom control (25%), reduced SE (20%), or combination of symptom control/SE (20%).
Conclusion: The use of directional stimulation at our center is similar to what is currently reported in the literature.2 We programmed with directional electrodes in ET more frequently compared to PD. This is likely because programming for a mono-symptomatic disorder is less complex and small differences are easier to identify which makes programming more time efficient. Moving forward testing directional stimulation in PD more routinely may be advantageous given the benefits and improvement in battery/TW% in our ET population.
References: 1. A. Schnitzler, P. Mir, M.A Brodsky, L. Verhagen, S. Groppa, R. Alvarez, A. Evans, M. Blazquez, S. Nagel, W. Libionka, J. Pilitsis, M. Pötter-Nerger, W. Tse, L. Almeida, N. Tomycz, J. Jimenez-Shahed, F. Carrillo, C.J Hartmann, S.J Groiss, F. Defresne, E. Karst, B. Cheeran, J. Vesper. Directional versus Omnidirectional Deep Brain Stimulation: Results of a Multicenter Prospective Blinded Crossover Study [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/directional-versus-omnidirectional-deep-brain-stimulation-results-of-a-multicenter-prospective-blinded-crossover-study/. Accessed March 8, 2021. 2. Ten Brinke TR, Odekerken VJJ, Dijk JM, van den Munckhof P, Schuurman PR, de Bie RMA. Directional deep brain stimulation: First experiences in centers across the globe. Brain Stimul. 2018;11(4):949-950.
To cite this abstract in AMA style:
J. Karl, J. Joyce, L. Verhagen Metman. Experience of DBS programming with directional leads [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/experience-of-dbs-programming-with-directional-leads/. Accessed December 15, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/experience-of-dbs-programming-with-directional-leads/