Objective: To investigate subgroup differences in the effect of COVID-19 stressors on mental health and quality of life in people with Parkinson’s disease.
Background: In order to facilitate tailored care for people with Parkinson’s disease, it is essential to identify subgroups that experienced the greatest impact of COVID-19 stressors on mental health and quality of life.
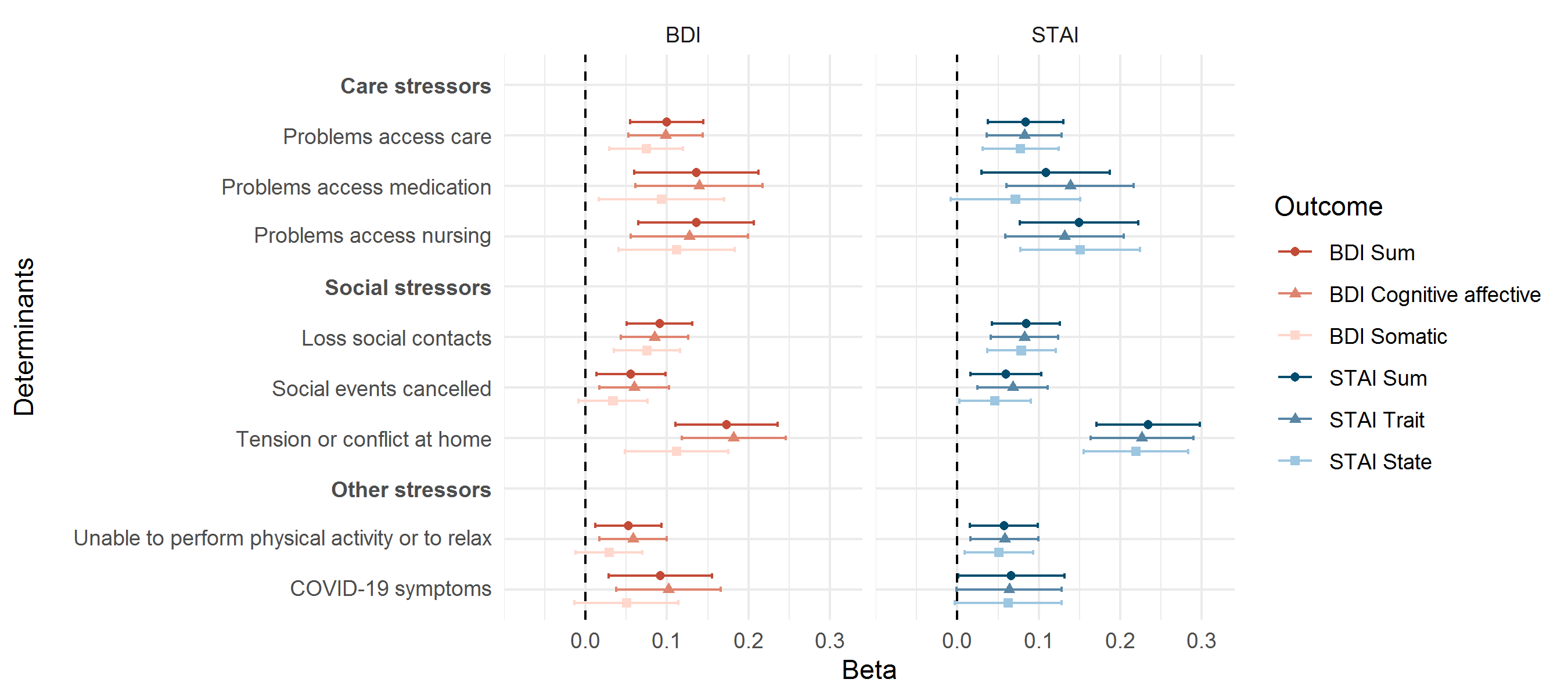
Method: This cross-sectional study uses baseline data of the PRIME-NL study. Eight COVID-19 stressors were summarized into care stressors, social stressors and a stressors sum score. Depression was measured with the Beck Depression Inventory (BDI), anxiety with the Spielberger State-Trait Anxiety Inventory (STAI) and quality of life with the Parkinson’s Disease Quality of Life Questionnaire (PDQ-39). The outcomes were standardized and models were adjusted for sex, age, years since diagnosis, presence of comorbidities, education, living situation and region. Stratifications were performed for demographics, disease-related and coping characteristics.
Results: The mean (SD) age of the 833 included participants was 70.2 (7.9) years and 317 (38.1%) participants were women. Higher COVID-19 stressors sum score was associated with worse depression (BDI beta: 0.03, 95% CI: 0.02-0.05), greater anxiety (STAI beta: 0.04, 95% CI: 0.02-0.05) and poorer quality of life (PDQ-39 beta: 0.03, 95% CI: 0.02-0.04). Figure 1 shows the associations between the eight individual stressors and BDI and STAI. Effects were apparent across subgroups, but larger in women, younger people, people with higher education, longer disease duration and higher MDS-UPDRS-II. Strata high in confrontive coping and planful problem solving showed smaller associations. An hypothetical intervention removing all eight COVID-19 stressors decreased BDI from 11.2 (95% CI: 10.7-11.6) to 9.0 (95% CI: 8.2-9.8), STAI from 74.3 (95% CI: 73.1-75.6) to 68.0 (95% CI: 65.4-70.5) and PDQ-39 from 25.1 (95% CI: 24.2-26.0) to 20.9 (95% CI: 19.3-22.6).
Conclusion: A broad range of COVID-19 stressors was associated with worse mental health and poorer quality of life across subgroups of people with Parkinson’s disease. Our results suggest that confrontive and planful problem solving coping strategies are beneficial. Our study highlights that COVID-19 stressors are important targets for tailored interventions to improve mental health in people with Parkinson’s disease during the COVID-19 pandemic.
To cite this abstract in AMA style:
L. Dommershuijsen, A. Heide, E. Berg, J. Labrecque, M K. Ikram, M A. Ikram, B. Bloem, R. Helmich, S. Darweesh. Effect of COVID-19 stressors on mental health and quality of life in Parkinson’s disease [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/effect-of-covid-19-stressors-on-mental-health-and-quality-of-life-in-parkinsons-disease/. Accessed April 3, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/effect-of-covid-19-stressors-on-mental-health-and-quality-of-life-in-parkinsons-disease/