Category: Parkinson's Disease: Pathophysiology
Objective: To find any relationship between cardiovascular risk factors such as diabetes mellitus, hypertension or both and worse state in patient with PD measured with the MDS-UPDRS I, II and IV subscales (with permission from the MDS).
Background: Parkinson disease (PD) is the second more prevalent neurodegenerative disease and cardiovascular risk factors have been associated to its development or progression, like diabetes mellitus and hypertension.
Method: We propose a study model trying to find any relation between these risk factors and worse state in patient with PD measured with the MDS-UPDRS I, II and IV subscales (with permission from the MDS).
We used I, II and IV subscales since they reflect closer reality to the state of the disease with respect to QOL, complications and ADL performance independent of on or off state.
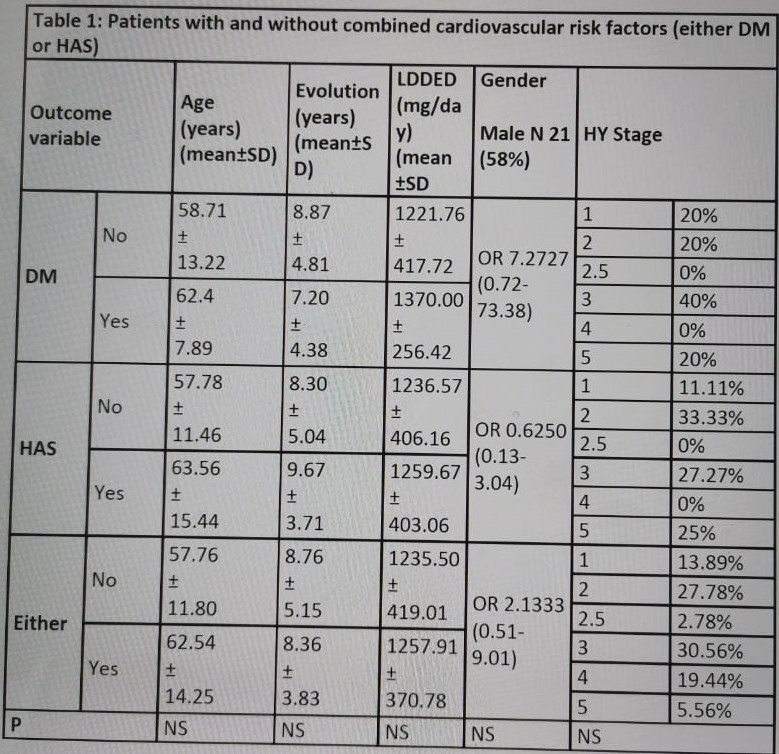
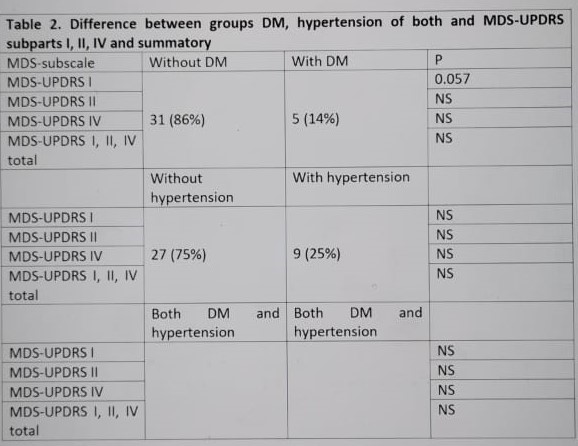
Results: We included 36 patients with Parkinson’s Disease 18 years-old and older, without functional surgery for PD. Patients signed out an informed consent to participate in our research. A survey was applied with demographical variables including the MDS-UPDRS subscales I, II and III for each patient. For study purposes we divided patients into groups with or without DM, hypertension or either, to analyze data.
We found 41.7% (15) females and 58.3% (21) males, with a mean of age of 59.22 ± 12.59, age of first symptom was 50.58 ±11.64 within 8.64 ± 4.73 years with diagnose of PD without statistical significance between patients stratified by gender or vascular risk factors (DM, hypertension, or any). We found 13.9% (5) patients with DM and 25% (9) patients with hypertension in our sample.
They showed marginal significative statistical difference with a higher score of the MDS-UPDRS-III for patients with PD and DM (P = 0.057).
Conclusion: In our study a confounder factor could be the known assotiaton to DM with cognitive and non-motor symptoms due to polyneuropathy icreasing the MDS-UPDRS-I score, however, mean time diagnosis with DM in our patients was less than 5 years and then not clinicaly strong to consider it as a confounder. In a post-hoc analysis the greater relation with worse MDS-UPDRS IV was with age of the patients and this variable needs to be consider for further studies.
References: 1. Wu Y, Le W, Jankovic J. Preclinical biomarkers of Parkinson disease. Arch Neurol. 2011 Jan;68(1):22-30. doi: 10.1001/archneurol.2010.321. PMID: 21220674. 2. Semchuk KM, Love EJ, Lee RG. Parkinson’s disease: a test of the multifactorial etiologic hypothesis. Neurology. 1993 Jun;43(6):1173-80. doi: 10.1212/wnl.43.6.1173. PMID: 8170564. 3. Schapira AH. Etiology and pathogenesis of Parkinson disease. Neurol Clin. 2009 Aug;27(3):583-603, v. doi: 10.1016/j.ncl.2009.04.004. PMID: 19555823. 4. Yue X, Li H, Yan H, Zhang P, Chang L, Li T. Risk of Parkinson Disease in Diabetes Mellitus: An Updated Meta-Analysis of Population-Based Cohort Studies. Medicine (Baltimore). 2016 May;95(18):e3549. doi: 10.1097/MD.0000000000003549. PMID: 27149468; PMCID: PMC4863785. 5. Yue X, Li H, Yan H, Zhang P, Chang L, Li T. Risk of Parkinson Disease in Diabetes Mellitus: An Updated Meta-Analysis of Population-Based Cohort Studies. Medicine (Baltimore). 2016 May;95(18):e3549. doi: 10.1097/MD.0000000000003549. PMID: 27149468; PMCID: PMC4863785. 6. Bohnen NI, Kotagal V, Müller ML, Koeppe RA, Scott PJ, Albin RL, Frey KA, Petrou M. Diabetes mellitus is independently associated with more severe cognitive impairment in Parkinson disease. Parkinsonism Relat Disord. 2014 Dec;20(12):1394-8. doi: 10.1016/j.parkreldis.2014.10.008. Epub 2014 Oct 15. PMID: 25454317; PMCID: PMC4314515. 7. Chang YH, Yen SJ, Chang YH, Wu WJ, Lin KD. Pioglitazone and statins lower incidence of Parkinson disease in patients with diabetes mellitus. Eur J Neurol. 2021 Feb;28(2):430-437. doi: 10.1111/ene.14542. Epub 2020 Oct 25. PMID: 32969141. 8. Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, Rascol O, Schrag A, Teresi JA, van Hilten JJ, LaPelle N; Movement Disorder Society UPDRS Revision Task Force. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008 Nov 15;23(15):2129-70. doi: 10.1002/mds.22340. PMID: 19025984. 9. Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P. Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol. 2006 Jan;5(1):64-74. doi: 10.1016/S1474-4422(05)70284-2. Erratum in: Lancet Neurol. 2006 Feb;5(2):113. PMID: 16361024. 10. Biessels GJ, Strachan MW, Visseren FL, Kappelle LJ, Whitmer RA. Dementia and cognitive decline in type 2 diabetes and prediabetic stages: towards targeted interventions. Lancet Diabetes Endocrinol. 2014 Mar;2(3):246-55. doi: 10.1016/S2213-8587(13)70088-3. Epub 2013 Oct 18. PMID: 24622755. 11. Verdile G, Fuller SJ, Martins RN. The role of type 2 diabetes in neurodegeneration. Neurobiol Dis. 2015 Dec; 84:22-38. doi: 10.1016/j.nbd.2015.04.008. Epub 2015 Apr 26. PMID: 25926349.
To cite this abstract in AMA style:
H. Gonzalez-Usigli, A. Gonzalez-Vazquez, J. Garcia-Rivera, O. Padila-Delatorre, A. Leon-Gil, H. Gonzalez-Rodriguez. Comparative score on the MDS-UPDRS scale I, II and IV in patients with Parkinson disease with and without cardiovascular risk factors. [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/comparative-score-on-the-mds-updrs-scale-i-ii-and-iv-in-patients-with-parkinson-disease-with-and-without-cardiovascular-risk-factors/. Accessed January 7, 2026.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/comparative-score-on-the-mds-updrs-scale-i-ii-and-iv-in-patients-with-parkinson-disease-with-and-without-cardiovascular-risk-factors/