Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To assess whether repeat olfactory testing in initially hyposmic subjects improves prediction of conversion to Parkinson disease (PD).
Background: Hyposmia is a common prodromal feature of PD, often predating clinical diagnosis by years1. As a result, olfactory testing has been proposed as a screening tool, given its low cost and ease of completion. Hyposmia is sensitive for the development of PD, but lacks specificity2. In this study we assess whether repeat smell testing improves its diagnostic characteristics for predicting conversion to PD in a community cohort.
Method: Participants completed up to 12 years of clinical and imaging evaluations as part of PARS3. Olfaction was assessed with the University of Pennsylvania Smell Identification Test (UPSIT), where accuracy less than the 15th percentile of age and gender norms was considered hyposmic. Subjects who completed 2 smell tests without clinical or imaging evidence of PD prior to the 2nd test were included (n=243). Development of PD was defined as clinical diagnosis on annual assessments or DAT deficit (less than 65% of age-expected lowest putamen specific binding ratio) on [123I] β-CIT SPECT scans completed approximately every two years. Kaplan Meier (KM) survival analysis and Cox proportional hazards regression (Cox) were used to estimate the hazard ratio for developing PD based on olfactory testing.
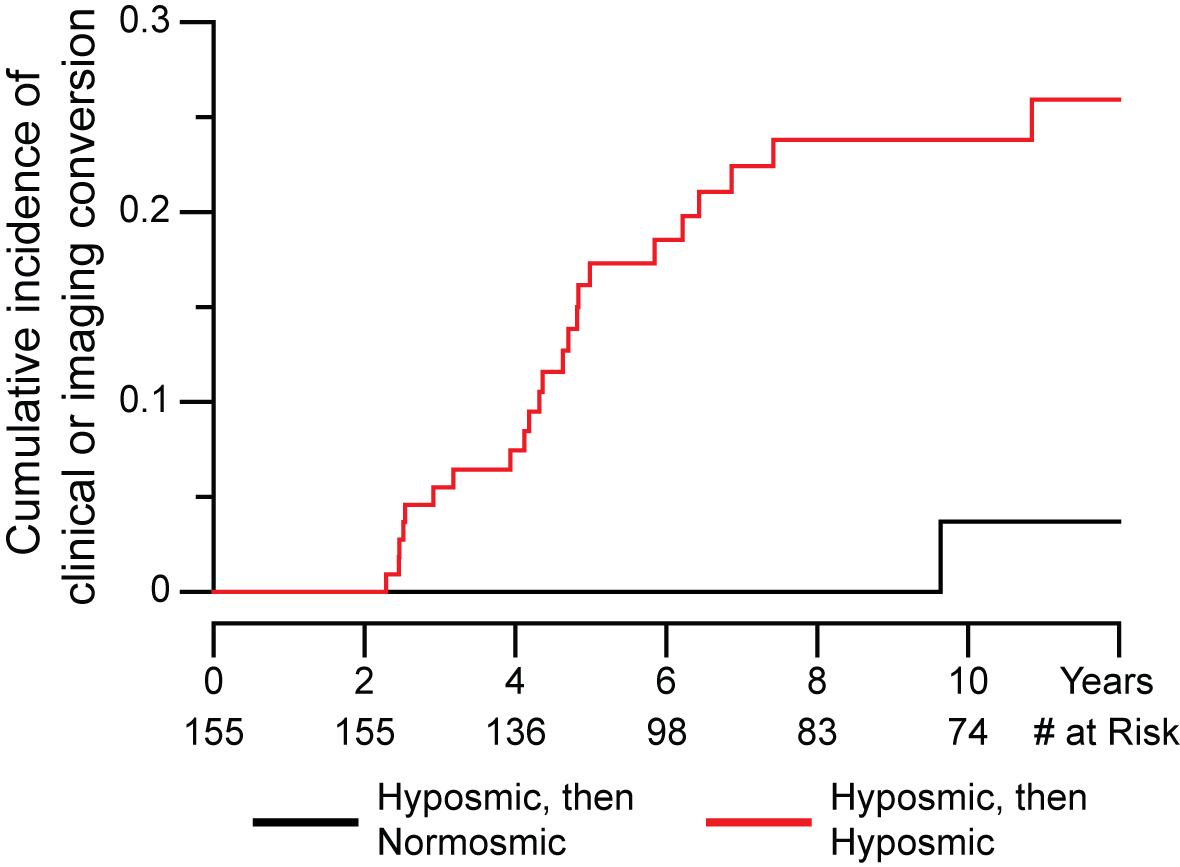
Results: Repeat olfactory testing was completed on average 1.4±0.5 years after the baseline smell test. 46 of 155 (30%) participants who were hyposmic at baseline reverted to normosmia. 23 of 109 (21%) of subjects with consistent hyposmia on baseline and repeat testing had evidence of conversion to PD, compared with 0 of 88 initially normosmic participants and 1 of 46 (2%) of initially hyposmic participants who reverted. Sensitivity and specificity for a single test were 100% and 40% and for consistent hyposmia were 96% and 61%, respectively. KM curves are shown in [figure1]. In Cox regression models accounting for age, sex, baseline UPDRS, and other nonmotor features, the hazard ratio for developing PD between consistent hyposmia and reversion was 10.0 (95% CI 1.3-75.8, p=0.03).
Conclusion: Serial smell testing improves detection of prodromal PD compared to a single test. Repeat testing may be an efficient and cost-effective strategy to identify at-risk patients for early diagnosis and disease modification studies.
References: 1. Ross GW, Petrovitch H, Abbott RD, et al. Association of olfactory dysfunction with risk for future Parkinson’s disease. Ann Neurol. 2008;63(2):167-173. doi:10.1002/ana.21291 2. Morley JF, Cohen A, Silveira-Moriyama L, et al. Optimizing olfactory testing for the diagnosis of Parkinson’s disease: item analysis of the university of Pennsylvania smell identification test. npj Park Dis. 2018;4(1). doi:10.1038/s41531-017-0039-8 3. Siderowf A, Jennings D, Stern M, et al. Clinical and Imaging Progression in the PARS Cohort: Long-Term Follow-up. Mov Disord. 2020;35(9):1550-1557. doi:10.1002/mds.28139
To cite this abstract in AMA style:
P. Vaswani, J. Morley, D. Jennings, A. Siderowf, K. Marek, P. Investigators. Serial olfactory testing for the diagnosis of prodromal Parkinson disease in the Parkinson Associated Risk Syndrome (PARS) study [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/serial-olfactory-testing-for-the-diagnosis-of-prodromal-parkinson-disease-in-the-parkinson-associated-risk-syndrome-pars-study/. Accessed April 2, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/serial-olfactory-testing-for-the-diagnosis-of-prodromal-parkinson-disease-in-the-parkinson-associated-risk-syndrome-pars-study/