Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To test whether structural pathology of the locus coeruleus (LC) is associated with orthostatic hypotension (OH) in Parkinson disease (PD).
Background: OH is an often debilitating PD symptom, but its mechanism has not been clarified. A potential role for LC degeneration in OH is unexamined in humans. We used neuromelanin-sensitive MRI to compare LC volumes between PD patients with and without OH within one minute of standing (immediate OH, iOH). We then looked for correlations between LC volume and orthostatic vital signs (OVS). Because OH is associated with cognitive decline we also tested for correlations with cognition (Montreal Cognitive Assessment, MoCA).
Method: The Unified Parkinson’s Disease Rating Scale Part III Motor Exam (UPDRS-III), MoCA, and OVS (supine vs. active standing) were collected in 62 early to moderate PD patients in the ON-medication state. Neuromelanin-sensitive MRI data were acquired with two Siemens 3T MRI scanners (Trio, Prisma-fit) using a 2D gradient echo sequence with magnetization transfer preparation pulse. LC and substantia nigra pars compacta (SNc) volumes were determined using a highly reproducible approach robust to scanner type (Langley et al, 2016). Demographics, UPDRS-III, MoCA, and OVS were compared in PD with iOH vs. without iOH using Chi-square testing or analysis of variance as appropriate. Multivariate analysis of covariance (covariates: supine heart rate (sHR), UPDRS-III, age) evaluated LC/SNc volume differences between groups. Partial correlations (covariates: scanner type, age; one-tailed) with false discovery rate correction (FDR) were assessed between LC volume-OVS and LC volume-MoCA.
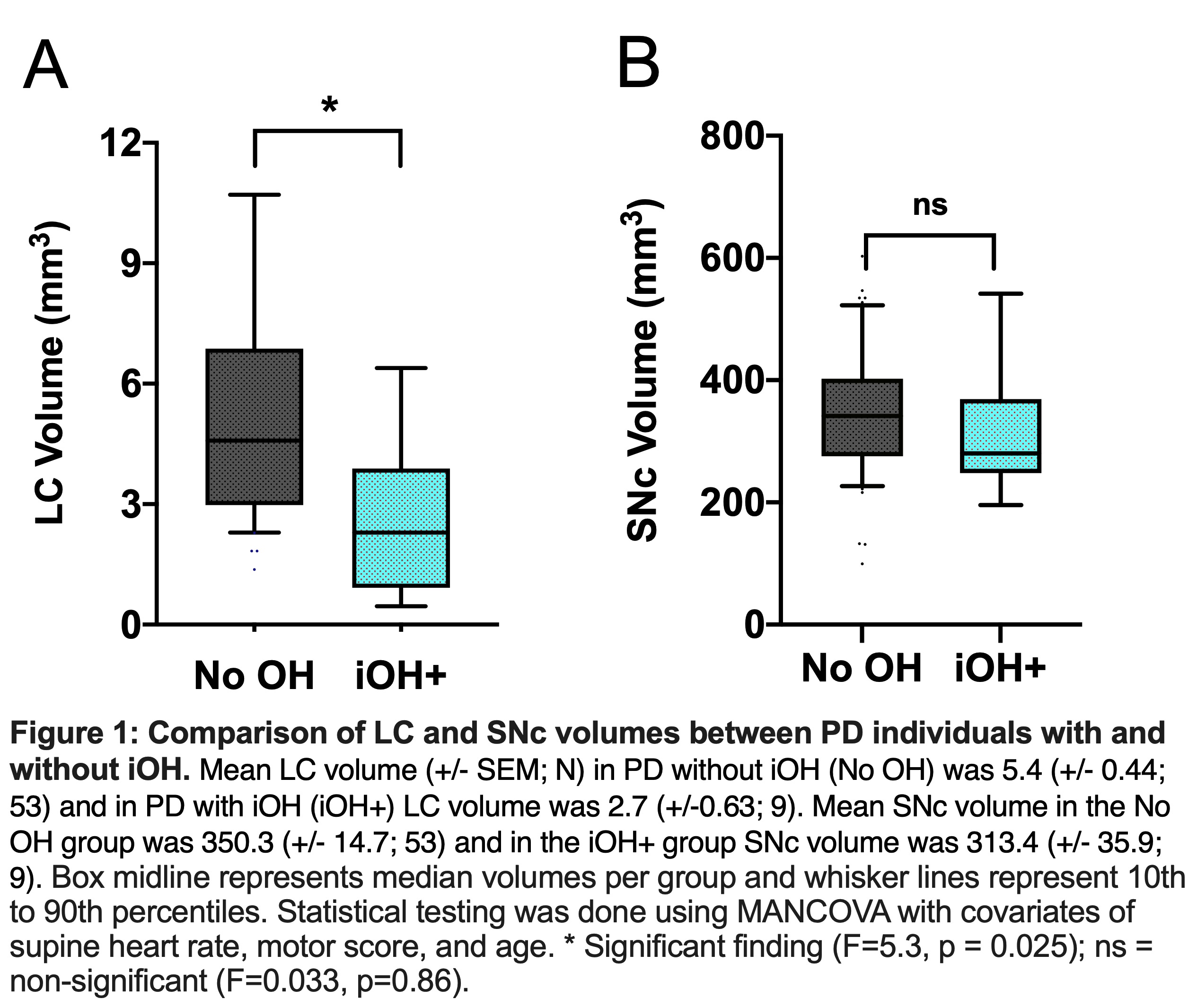
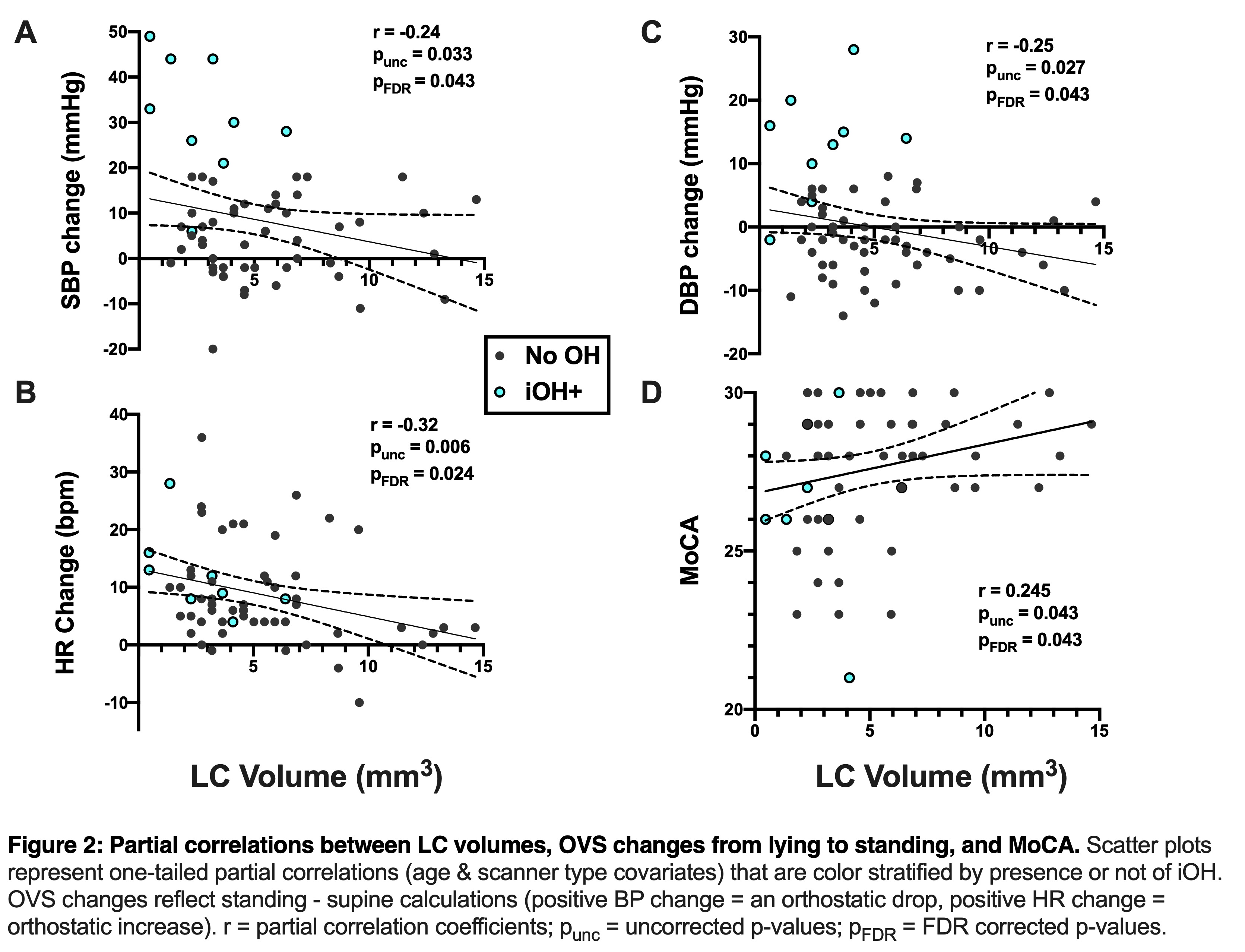
Results: PD with and without iOH did not differ significantly based on demographics, disease duration, levodopa equivalent doses, UPDRS-III, or MoCA (p>0.05). LC, but not SNc, volume was significantly reduced in PD with iOH (N=9) vs. without OH (N=53; LC p=0.013; SNc p=0.76; Fig 1.). LC volumes correlated with all OVS measures (N=62; systolic blood pressure r = -0.24, pFDR = 0.043, Fig 2A; diastolic blood pressure r = -0.25, pFDR = 0.043, Fig 2B; sHR r = -0.32, pFDR = 0.024, Fig 2C). LC volume also correlated with MoCA score (r = 0.25, pFDR = 0.043, Fig 2D).
Conclusion: This study suggests that LC pathology may be a neural substrate for both OH and cognitive decline in PD. A larger cohort of OH patients should be studied to help validate these findings.
References: Langley, J., Huddleston, D.E., Liu, C.J. et al. Reproducibility of locus coeruleus and substantia nigra imaging with neuromelanin sensitive MRI. Magn Reson Mater Phy 30, 121–125 (2017). https://link.springer.com/article/10.1007/s10334-016-0590-z
To cite this abstract in AMA style:
P. Beach, N. Kurra, K. Hwang, J. Langley, X. Hu, D. Huddleston. Locus coeruleus volume is reduced in Parkinson disease-related orthostatic hypotension. [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/locus-coeruleus-volume-is-reduced-in-parkinson-disease-related-orthostatic-hypotension/. Accessed March 31, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/locus-coeruleus-volume-is-reduced-in-parkinson-disease-related-orthostatic-hypotension/