Category: Parkinson's Disease: Neuroimaging
Objective: To investigate the association between brainstem planimetry and REM behaviour disorder (RBD) in de novo Parkinson’s disease (PD).
Background: RBD is associated with a prominent volume loss in the latero-dorsal tegmental nucleus, situated in the brainstem, spanning the midbrain and the pontine tegmentum where cholinergic, GABAergic and glutamatergic neurons are located and implicated in the promotion of REM sleep and muscle atonia (1). MRPI was introduced as an improvement on the simpler midbrain to pons area ratio (M/P), and take into account also middle and superior cerebellar peduncle width ratio (2).
Method: Data on 214 de novo PD patients were obtained from the Parkinson’s Progression Markers Initiative (PPMI). The probable presence or absence of RBD in PD patients was based on RBD screening questionnaire. PD patients with a RBDSQ score ≥ 5 were considered as probable RBD (RBD-PD). Data extracted included demographics, motor assessment and [123I]FP-CIT SPECT scan to assess dopaminergic striatal denervation. Volumetric 3T T1-weighted MR images were used for morphological calculations. Chi-squared test and ANCOVA assessed the differences between groups. Multiple linear regression model was used to explore correlation between RBDSQ and MRPI. The analyses were adjusted for age and sex.
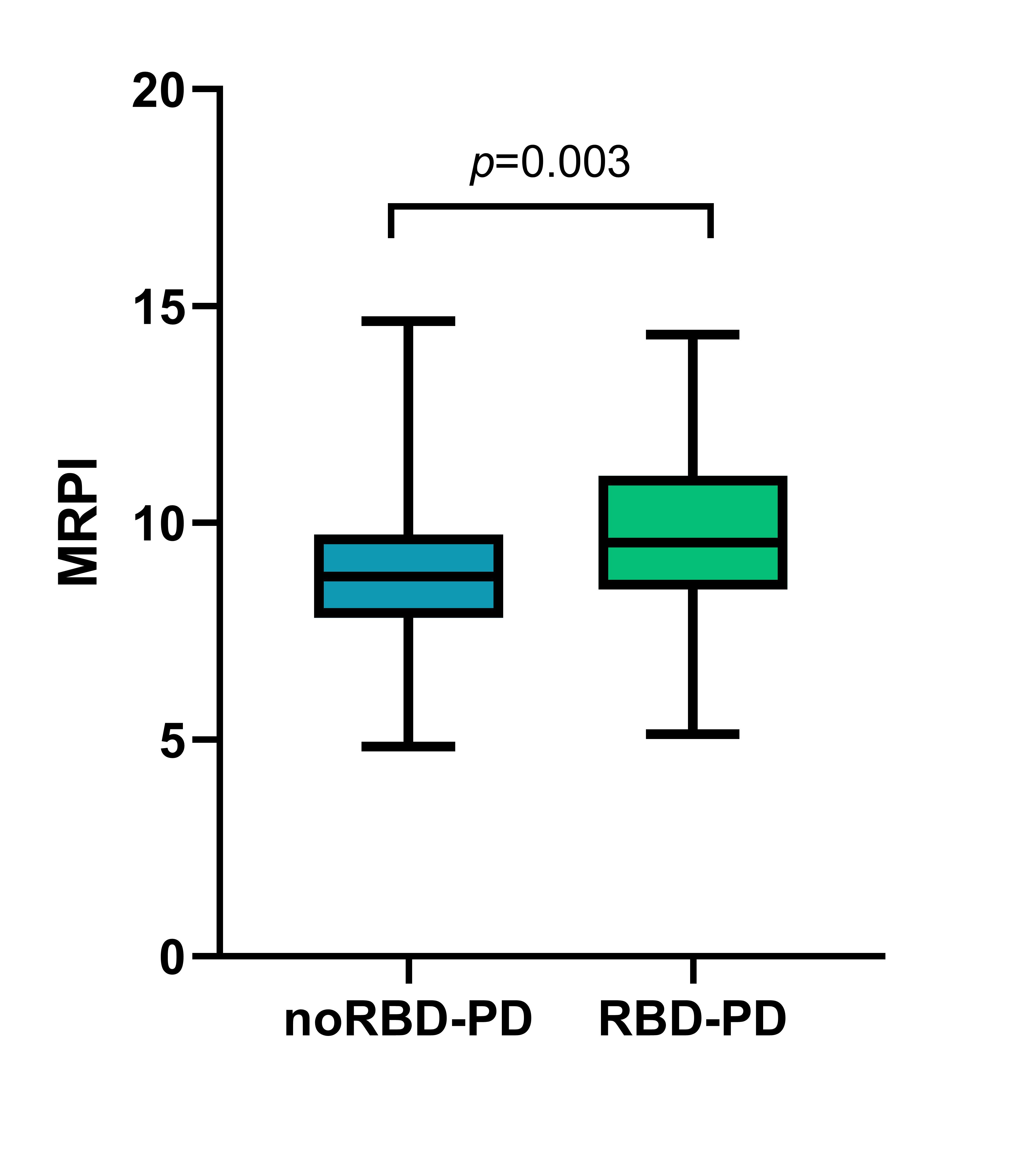
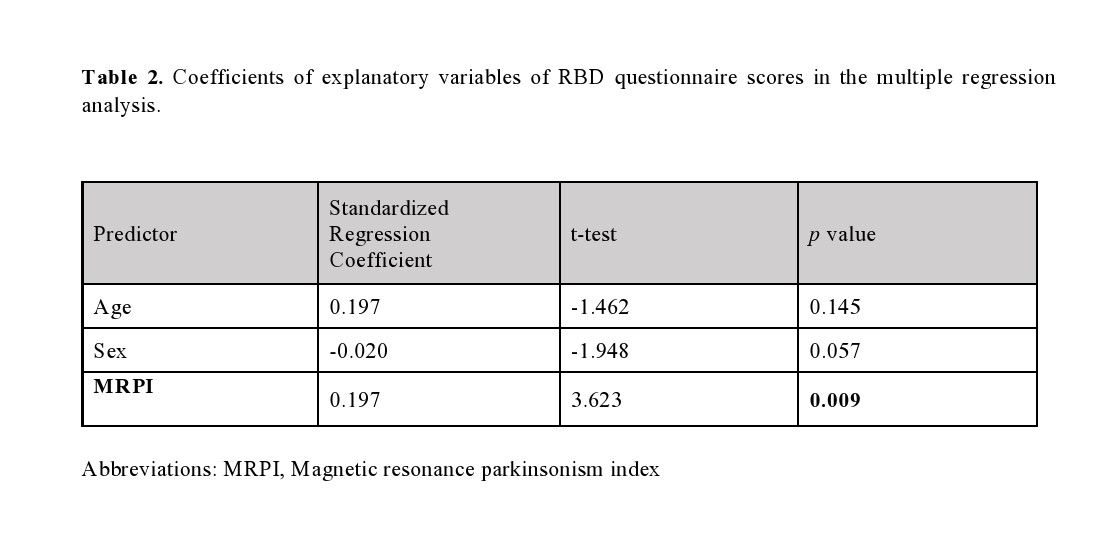
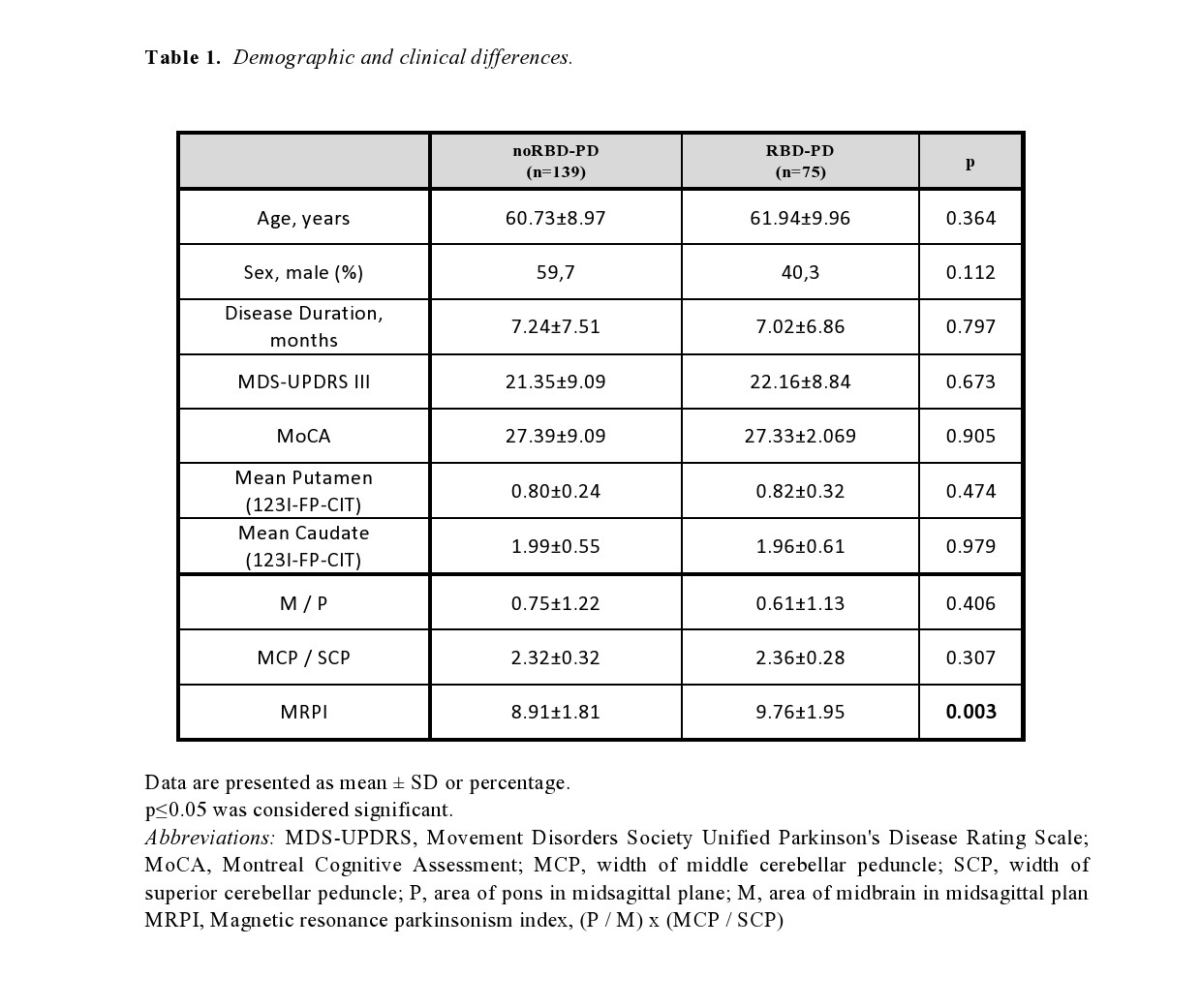
Results: Seventy-five PD patients were classified as RBD-PD while 139 as noRBD-PD. Clinical data of the groups were compared and are illustrated in Table 1. There were no significant differences in demographic characteristics (age and sex), motor burden (MDS-UPDRS), cognitive impairment (MoCA), and striatal biding ratio in the putamen and caudate (123I-FP-CIT). MRPI was higher in the RBD-PD group (p=0.003, Figure 1) compared with the noRBD-PD group. No differences were found in other morphometric ratios. In the multiple linear regression model, MRPI was a significant predictor of RBDSQ scores (β=0.197, p=0.009, Table 2).
Conclusion: Our findings support that MRPI can be used as an imaging marker of RBD in patients with de novo PD.
References: 1. Boucetta S, Salimi A, Dadar M, Jones BE, Collins DL, Dang-Vu TT. Structural Brain Alterations Associated with Rapid Eye Movement Sleep Behavior Disorder in Parkinson’s Disease. Scientific Reports. 2016;6(1):26782. 2. Nigro S, Antonini A, Vaillancourt DE, et al. Automated MRI Classification in Progressive Supranuclear Palsy: A Large International Cohort Study. Movement Disorders. 2020;35(6):976-983.
To cite this abstract in AMA style:
D. Urso, S. Nigro, B. Tafuri, G. Logroscino. Brainstem planimetry in Parkinson’s disease with REM behaviour disorder. [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/brainstem-planimetry-in-parkinsons-disease-with-rem-behaviour-disorder/. Accessed February 6, 2026.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/brainstem-planimetry-in-parkinsons-disease-with-rem-behaviour-disorder/