Category: Parkinson's Disease: Neuroimaging
Objective: To compare the sensitivity of detection cortical degenerative changes in patients with Parkinson’s disease (PD) and mild cognitive impairment (MCI) between the diffusion magnetic resonance imaging (MRI) and structural MRI.
Background: Cognitive impairment is one of the most common and debilitating non-motor symptoms of PD. Early identifying PD-MCI, who are at higher risk with dementia, are clinical essential. Structural MRI reported regional cortical atrophy in PD-MCI with inconsistent results. Techniques sensitive to brain microstructure may be better suited to detect cortical changes linked to PD-MCI.
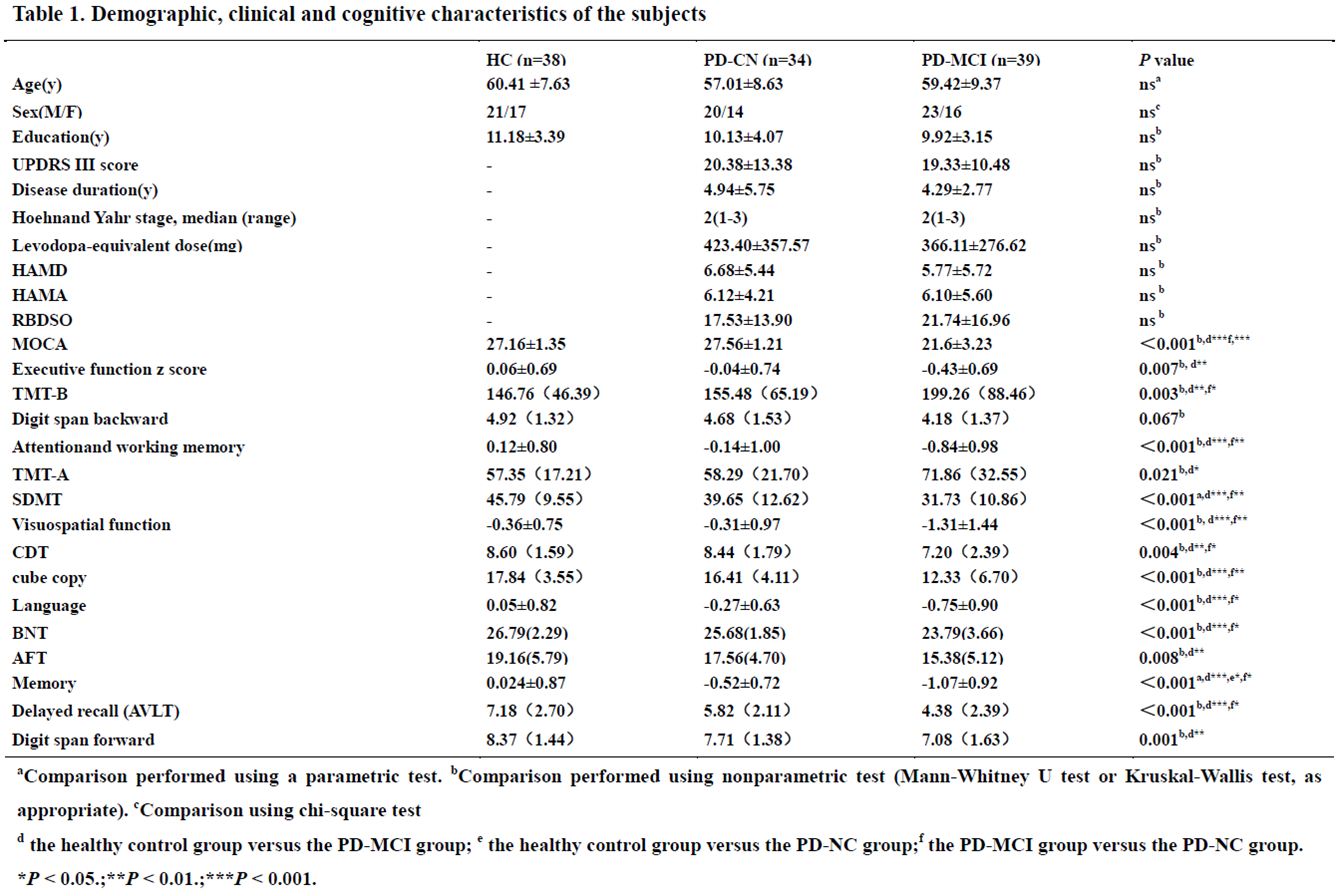
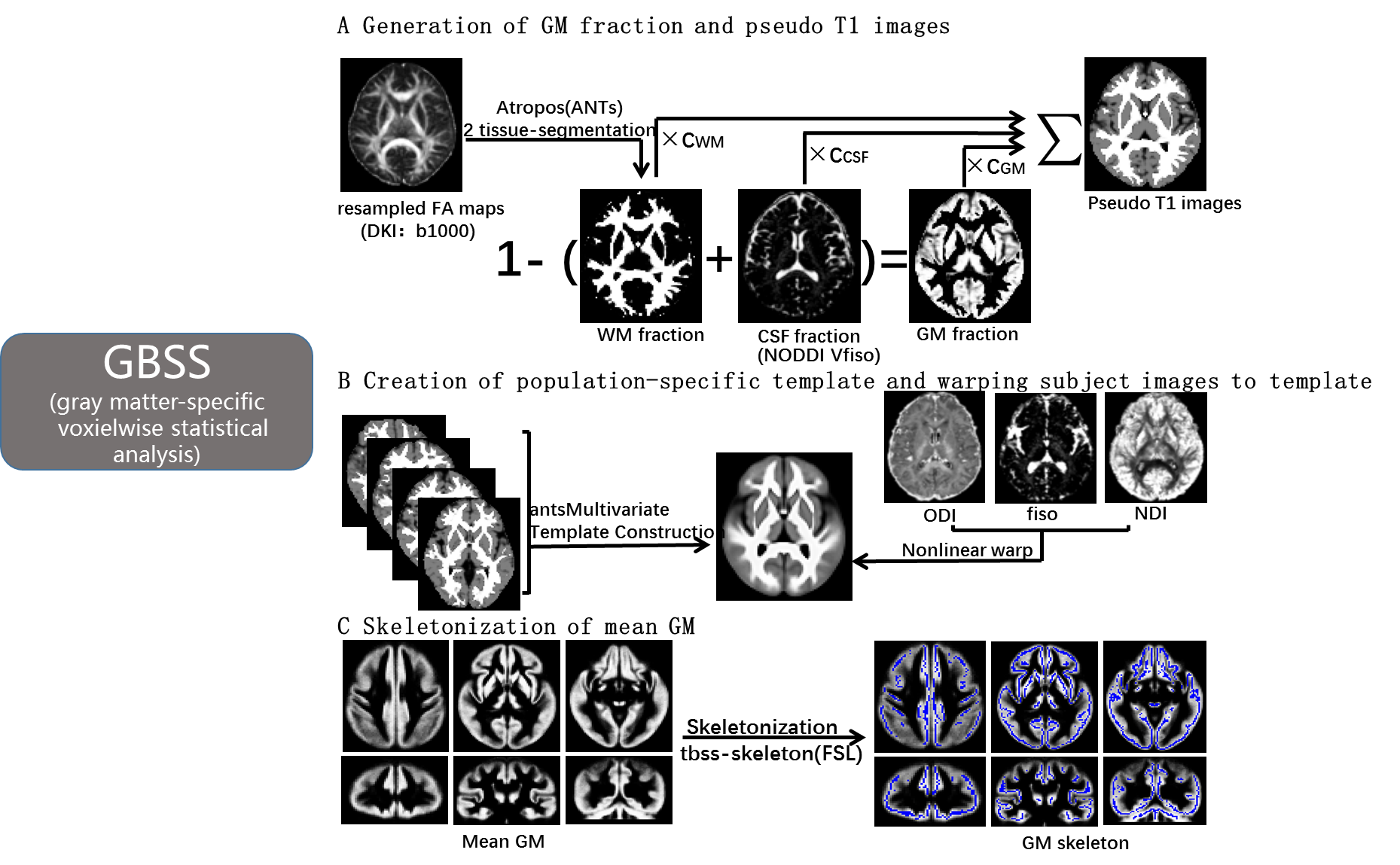
Method: A total of 111 subjects, including 34 patients with normal cognition (PD-CN), 39 PD-MCI, and 38 healthy controls (HC), were included. PD-MCI was diagnosed according to the MDS Task Force level 2 criteria. Cortical microstructural alterations were evaluated by using Neurite Orientation Dispersion and Density Imaging (NODDI) model with gray matter-based spatial statistics (GBSS) (Figure 1). Cortical thickness analyses were performed using the FreeSurfer software.
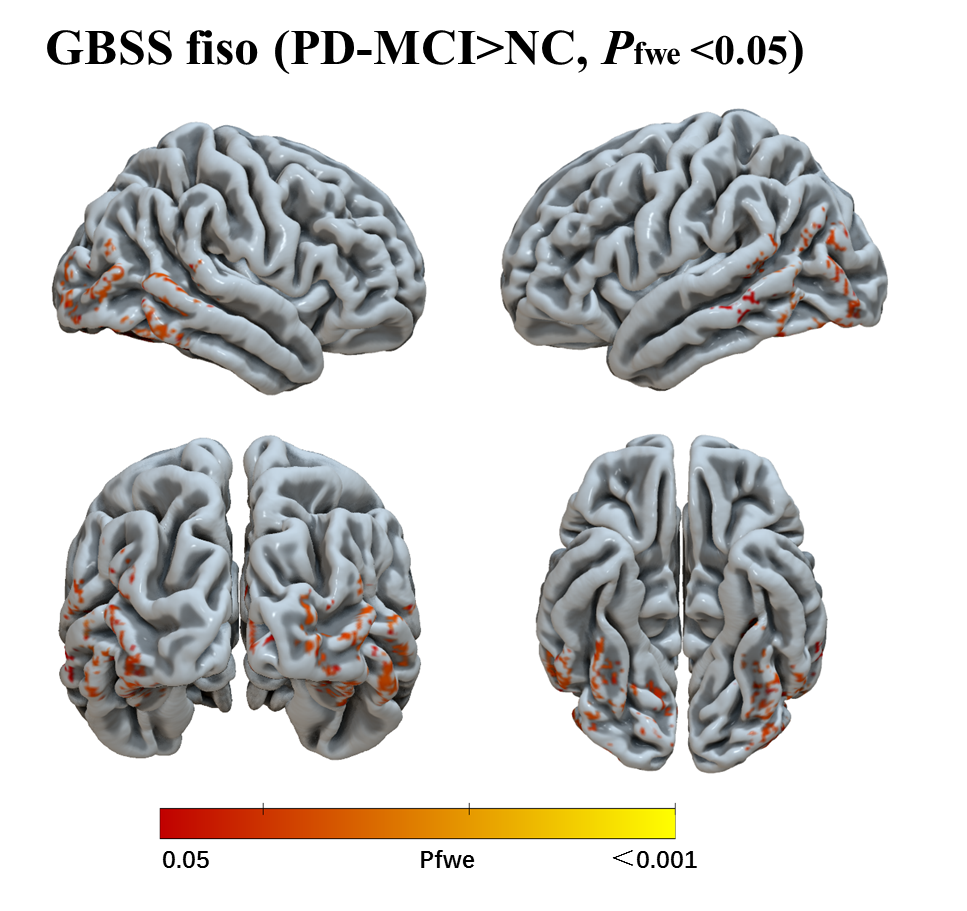
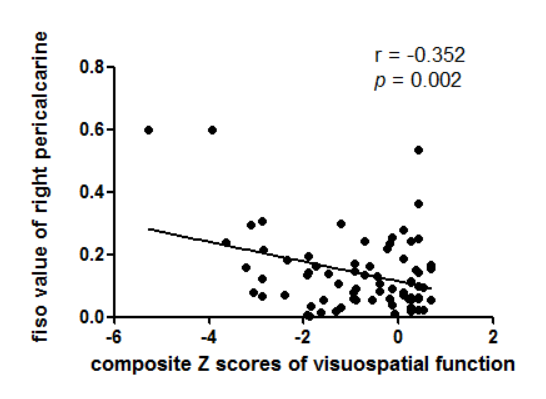
Results: The demographic and clinical characteristics of all subjects are presented in Table 1. For cortical microstructural analyses, compared with HC, PD-MCI showed significantly higher volume fraction of isotropic diffusion (fiso) predominantly in the posterior cortices, including the bilateral temporal lobe, fusiform,inferior parietal, lateral occipital, and parahippocampal, and left supramarginal, and right cuneus, right lingual, and right pericalcarine (Figure 2), while there was no difference of neurite density index (NDI) or orientation dispersion index (ODI). No significant difference was found between the PD-MCI group and the PD-CN group or between the PD-CN group and the HC group for cortical microstructural alterations. For cortical thickness analyses, there were no group difference in any vertex in the between-group comparisons. The fiso values of right pericalcarine was associated with the visuospatial cognitive function in the PD patients (r = – 0.352, p=0.002) ( Figure 3).
Conclusion: Our results suggest that cortical microstructural alterations may be much more sensitive than morphology changes to cortical degeneration in PD-MCI.
References: [1]. Janvin C C, Larsen J P, Aarsland D, Hugdahl K (2006) Subtypes of mild cognitive impairment in parkinson’s disease: Progression to dementia. Movement Disorders 9:1343-1349. [2]. Melzer T R, Watts R, MacAskill M R et al (2012) Grey matter atrophy in cognitively impaired Parkinson’s disease. J Neurol Neurosurg Psychiatry 2:188-194. [3]. Pereira J B, Svenningsson P, Weintraub D et al (2014) Initial cognitive decline is associated with cortical thinning in early Parkinson disease. Neurology 22:2017-2025. [4]. Thomas G E C, Leyland L A, Schrag A-E, Lees A J, Acosta-Cabronero J, Weil R S (2020) Brain iron deposition is linked with cognitive severity in Parkinson’s disease. Journal of Neurology, Neurosurgery & Psychiatry 4:418-425. [5]. Sampedro F, Martinez-Horta S, Marin-Lahoz J, Pagonabarraga J, Kulisevsky J (2019) Longitudinal intracortical diffusivity changes in de-novo Parkinson’s disease: A promising imaging biomarker. Parkinsonism Relat Disord:22-25.
To cite this abstract in AMA style:
X. Bai, T. Guo, X. Guan, C. Zhou, J. Wu, M. Zhang. Cortical microstructural alterations are more sensitive than morphology changes to cortical degeneration in Parkinson’s disease with mild cognitive impairment [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/cortical-microstructural-alterations-are-more-sensitive-than-morphology-changes-to-cortical-degeneration-in-parkinsons-disease-with-mild-cognitive-impairment/. Accessed February 3, 2026.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/cortical-microstructural-alterations-are-more-sensitive-than-morphology-changes-to-cortical-degeneration-in-parkinsons-disease-with-mild-cognitive-impairment/