Category: Parkinson's Disease: Cognitive functions
Objective: This study aimed to assess the incidence of falls in a population of PD patients and their clinical performance on cognitive assessment scales.
Background: Parkinson’s Disease (PD) gait impairment and falls are associated with an interface between motor dysfunction and cognitive decline, mainly in executive function and attention domains.(1) Formal education directly affects performance in executive function assessment batteries. Patients with lower educational levels usually have worse performance on cognitive and motor assessment scales.(2,3,4)
Method: Cross-sectional evaluation of demographic and clinical data from PD patients from a Movement Disorder Center in Fortaleza, Ceara, Brazil.
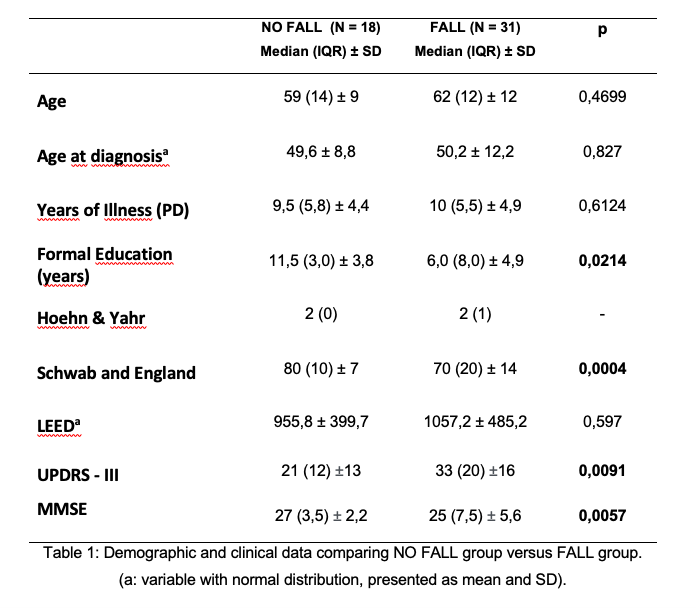
Results: We evaluated 49 PD patients, predominantly male (67%) with average age of 59 years (±10,9). Thirty-one patients (63.2%) experienced at least one fall episode in the last year and 86% (N=42) experienced a near-fall situation. We observed a homogeneous distribution between fall and no-fall groups regarding to age, age at diagnosis and years of illness. There was no statistical difference between LEED used (p = 0.597). Individuals on fall group had worse overall performance on UPDRS part III (table 1) and greater impairment in the perception of performance of ADLs by Schwab and England (p = 0.0004). This may reflect a greater motor impairment and a greater degree of dependence in fall group, factors related to worse functional performance and with greater impact on quality of life. Patients in fall group obtained lower scores on Mini-Mental State Examination with worse performance in the execution of the pentagon drawing test. PD gait impairment is associated with the interface between motor dysfunction and cognitive impairment, mainly in executive function and attention. (1) Poor performance in cognitive tests in falls group, both in global scores and executive function scales, reinforces the cognitive reserve theory. The higher the educational level, more efficient and flexible neuronal circuitry connections are, compensating possible cognitive and motor deficiencies in neurodegenerative process.(6)
Conclusion: PD patients with history of falls presented with greater motor impairment and worse cognitive performance. As already known, impaired attention and executive function may exacerbate the difficulties in activities of daily living and contribute to recurrency of falls, with impact on quality of life.
References: 1. MIRELMAN, Anat et al. Gait impairments in Parkinson’s disease. The Lancet Neurology, v. 18, n. 7, p. 697–708, 2019. 2. BARBOSA, Alessandra Ferreira et al. Gait, posture and cognition in Parkinson’s disease. Dement Neuropsychol, v. 10, n. 4, p. 280–286, 2016. 3. KIERZYNKA, Anna; KAŹMIERSKI, Radosław; KOZUBSKI, Wojciech. Educational level and cognitive impairment in patients with Parkinson disease. Neurologia i Neurochirurgia Polska, v. 45, n. 1, p. 24–31, 2011. 4. SOUZA, Carolina de Oliveira et al. Influence of educational status on executive function and functional balance in individuals with parkinson disease. Cognitive and Behavioral Neurology, v. 26, n. 1, p. 6–13, 2013. 5. PICCININI, Giulia et al. The impact of cognitive reserve on the effectiveness of balance rehabilitation in Parkinson’s disease. European Journal of Physical and Rehabilitation Medicine. [S.l: s.n.]. , 2018
To cite this abstract in AMA style:
F. Rolim, A. Gomes, V. Santos, D. Torres, F. Carvalho. Falls in Parkinson’s Disease: The Impact of Cognitive Performance [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/falls-in-parkinsons-disease-the-impact-of-cognitive-performance/. Accessed January 5, 2026.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/falls-in-parkinsons-disease-the-impact-of-cognitive-performance/