Category: Parkinsonism, Atypical: PSP, CBD
Objective: Introduction: Progressive supranuclear palsy (PSP) is a rare brain condition. It is predominantly a sporadic disease that occurs between 45 and 75 years of age, typically after the age of 40. We herein report a presentation of PSP in a 35-year-old male patient.
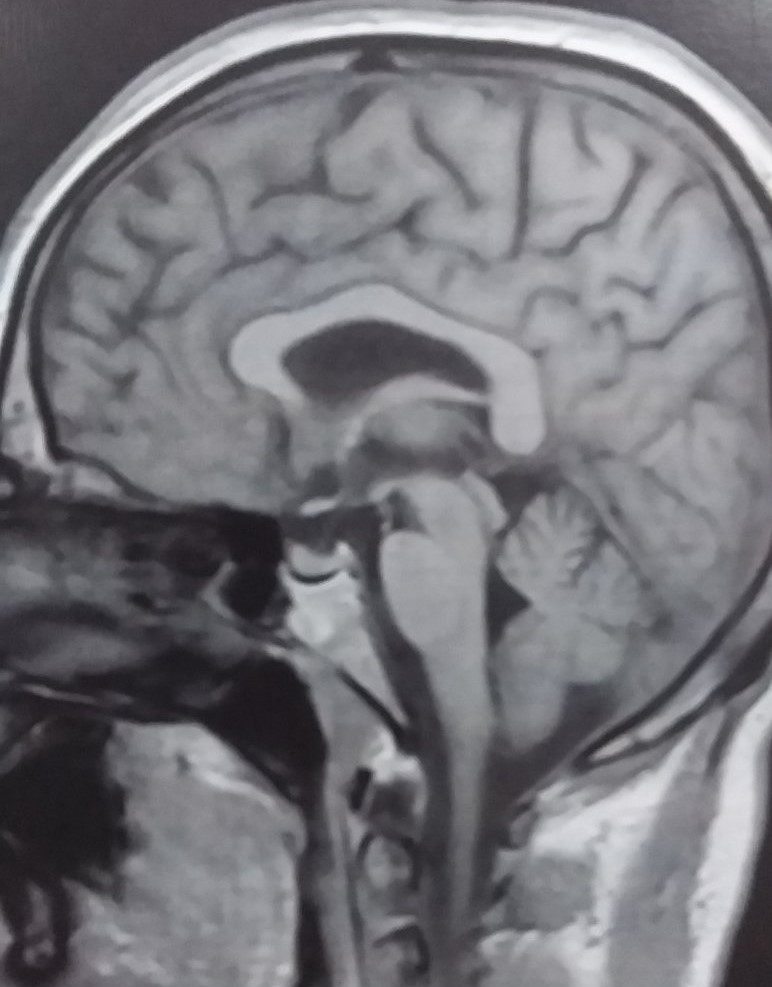
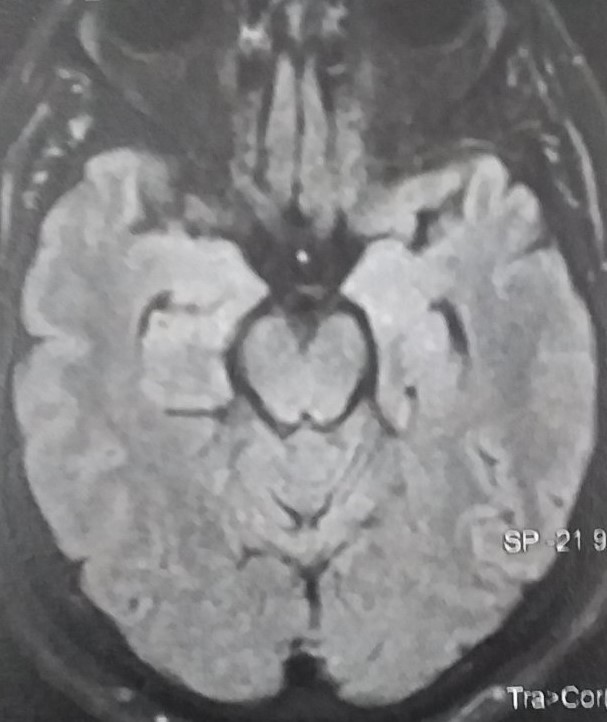
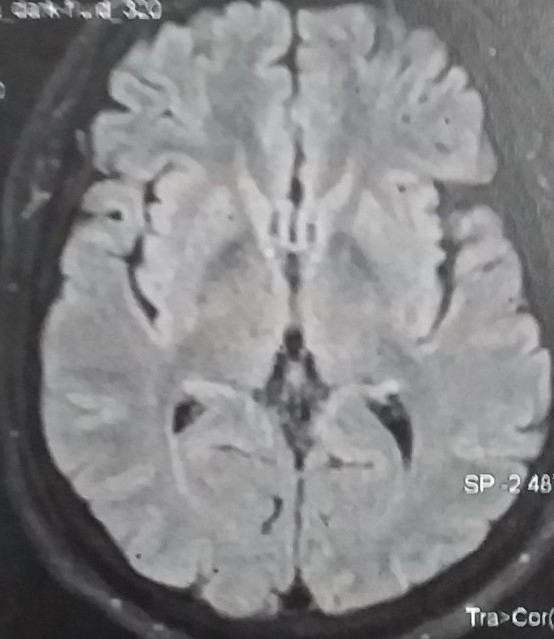
Background: Observation: A 35-year-old man progressively presented gait disturbances with postural instability leading to falls. On examination: Akineto-rigid parkinsonian syndrome (PS), primarily axial, associated with vertical gaze palsy, head backwards tilt and postural instability without tremor. There was a slight frontal syndrome, irritability and dysphagia. The biological assessment (autoimmunity, copper and CSF testing) was correct. Brain MRI of the onset [figure1] did not show mesencephalic atrophy, nor signal abnormalities of overload disorders (Wilson’s disease (WD), neuroferritinopathy). The patient underwent a therapeutic test (L-dopa 300 mg/d) over three months, without significant improvement.
We then added ropinirole, rivastigmine and paroxetine. Despite the given therapeutics, no remarkable changes were noticed.
Method: Discussion: PSP is the most common phenotype of parkinsonism after Parkinson’s disease (PD). Its prevalence estimated to be 5–7 cases /100 000 with peak occurrence at age 63 and no cases recorded before the age of 40. Although neuropathology is the gold standard for diagnosing definite PSP, certain clinical features, such as vertical supranuclear palsy evident in our patient are highly sensitive and specific. It is frequently seen in PSP and has strong relevance. A combination of clinical characteristics with high specificity is used to diagnose probable PSP. Vertical gaze palsy, pseudobulbar palsy, axial rigidity, falls and cognitive dysfunction are PSP’s clinical hallmarks.
Results: Our patient clinical presentation strongly suggested probable PSP with Richardson’s syndrome (PSP-RS), which is the commonest PSP presentations. In front of this atypical and sporadic PS, WD was ruled out as well as other differential diagnoses (anti-DPPX encephalitis). A control brain MRI is planned to look for possible midbrain atrophy that may not be found at the disease’s start. The patient clinical features are evocative arguments of the diagnosis, although the onset at the age of 35 is atypical and original.
Conclusion: Conclusion: The onset of PSP after the age of 40 is one of the diagnostic requirements so far, however, early presentations should be considered.
To cite this abstract in AMA style:
L. Megherbi, H. Si Ahmed, S. Daoudi. Unusual Progressive Supranuclear Palsy: a case report [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/unusual-progressive-supranuclear-palsy-a-case-report/. Accessed April 2, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/unusual-progressive-supranuclear-palsy-a-case-report/