Category: Parkinsonism, Atypical: MSA
Objective: To determine the effect of sleep position on morning OH in MSA patients
Background: Dysautonomia is considered as one of the most distress symptom in multiple system atrophy (MSA) patients. These include orthostatic hypotension (OH), supine hypertension (SH) and nocturnal hypertension (NH). SH and NH are the major limitations of the effective treatment of OH. The treatment strategies of OH usually worsening the SH and NH.
Method: This cross-sectional study enrolled 6 MSA patients and they were monitored 24-hours ambulatory blood pressure (ABPM) at their home during day- and night-time for two nights. Patients were instructed to sleep in the supine position for the entire first night and lateral position either right or left lateral for the entire second night. The additional BP measuring apart from the 30-min automated recording was assessed immediately after awakening in the morning in supine position followed by the 3-minute standing position. Morning OH was defined as the decrement of SBP ≥ 20 and /or DBP ≥ 10 mmHg, after 3-minute standing compared to supine position. SH was defined as SBP ≥ 140 and/or DBP ≥ 90 mmHg in supine position.
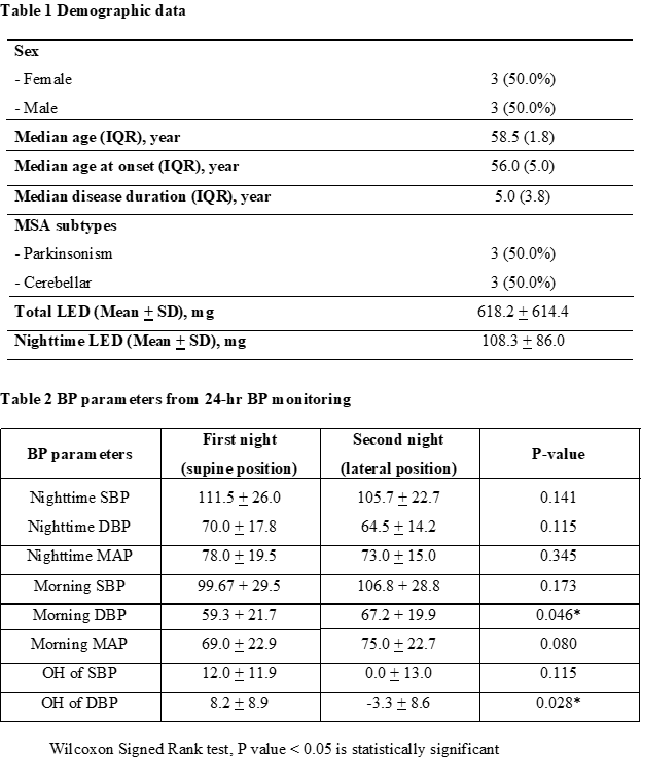
Results: There were 3 MSA-P and 3 MSA-C in this study. Other demographic data is shown in table 1. We found the significant difference between the mean morning DBP after sleeping with supine and lateral for the entire night (after sleeping in supine position was 59.3 + 21.7 mmHg vs after sleeping in lateral position was 67.2 + 19.9 mmHg, P= 0.046). In addition, the magnitude of OH in the morning was decrease significantly after sleeping in the lateral position for the entire night compared to after sleeping with supine position for the entire night (8.2 + 8.9 mmHg vs -3.3 + 8.6 mmHg, P=0.028). Other BP parameters are shown in table 2.
Conclusion: Our study demonstrated the effect of sleeping position in MSA patients. We found statistically significant difference of morning OH magnitude between sleeping in supine and lateral position. There was significantly more decrease in morning OH after sleeping in lateral position than in supine position. And thus, we proposed that sleep position might be a novel non-pharmacological treatment for MSA patients with OH in the morning.
References: – Fanciulli A, Strano S, Ndayisaba JP, Goebel G, Gioffre L, Rizzo M, et al. Detecting nocturnal hypertension in Parkinson’s disease and multiple system atrophy: proposal of a decision-support algorithm. J Neurol. 2014;261(7):1291-9. – Espay AJ, LeWitt PA, Hauser RA, Merola A, Masellis M, Lang AE. Neurogenic orthostatic hypotension and supine hypertension in Parkinson’s disease and related synucleinopathies: prioritisation of treatment targets. The Lancet Neurology. 2016;15(9):954-66. – Mendoza-Velásquez JJ, Flores-Vázquez JF, Barrón-Velázquez E, Sosa-Ortiz AL, Illigens BW, Siepmann T. Autonomic Dysfunction in α-Synucleinopathies. Front Neurol. 2019;10:363.
To cite this abstract in AMA style:
T. Prasertpan, J. Sringean, R. Bhidayasiri. The effect of sleep positions on morning orthostatic hypotension in Multiple System Atrophy patients: A pilot study [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/the-effect-of-sleep-positions-on-morning-orthostatic-hypotension-in-multiple-system-atrophy-patients-a-pilot-study/. Accessed April 3, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-effect-of-sleep-positions-on-morning-orthostatic-hypotension-in-multiple-system-atrophy-patients-a-pilot-study/