Category: Other
Objective: To assess the acceptability of virtual consultations as an option for out-patient clinic consultations for PD
Background: The practice of telemedicine increased dramatically on account of the global restrictions caused by the SARS CoV-2 pandemic. Disruptions in clinical services, and concerns for personal safety have had a significant impact on persons with PD who ordinarily require access to specialist care, are typically older and more dependent, and are a high-risk category for COVID. Viable options to ensuring continuity of care without compromising quality of care are desirable. Whereas adoption of virtual consultations may bridge this gap, variations to access exists between countries.
Method: This pre-implementation survey was developed to explore the acceptability and barriers to use of remote virtual consultations for follow up of PD, in preparation for a clinical trial. Approval of the survey protocol was obtained from each participating center’s IRB. The participating sites were located in Nigeria, Spain, Egypt, Tanzania, U.S.A, Uruguay Saudi Arabia, and South Korea, selected on the basis of MD expertise drawn from the TMSG of the MDS. The survey was deployed in consecutively attending persons with PD, with a target to include 40 PD per site. Interviews were face-to-face and conducted by a trained interviewer or the participating neurologist. Respondents were the person with PD and/or accompanying caregiver. In summary, survey included socio-demographic characteristics, questions about logistics of current clinic visits, disability on the Hoehn and Yahr scale, and questions addressing acceptability of virtual consultations and preferences for the format.
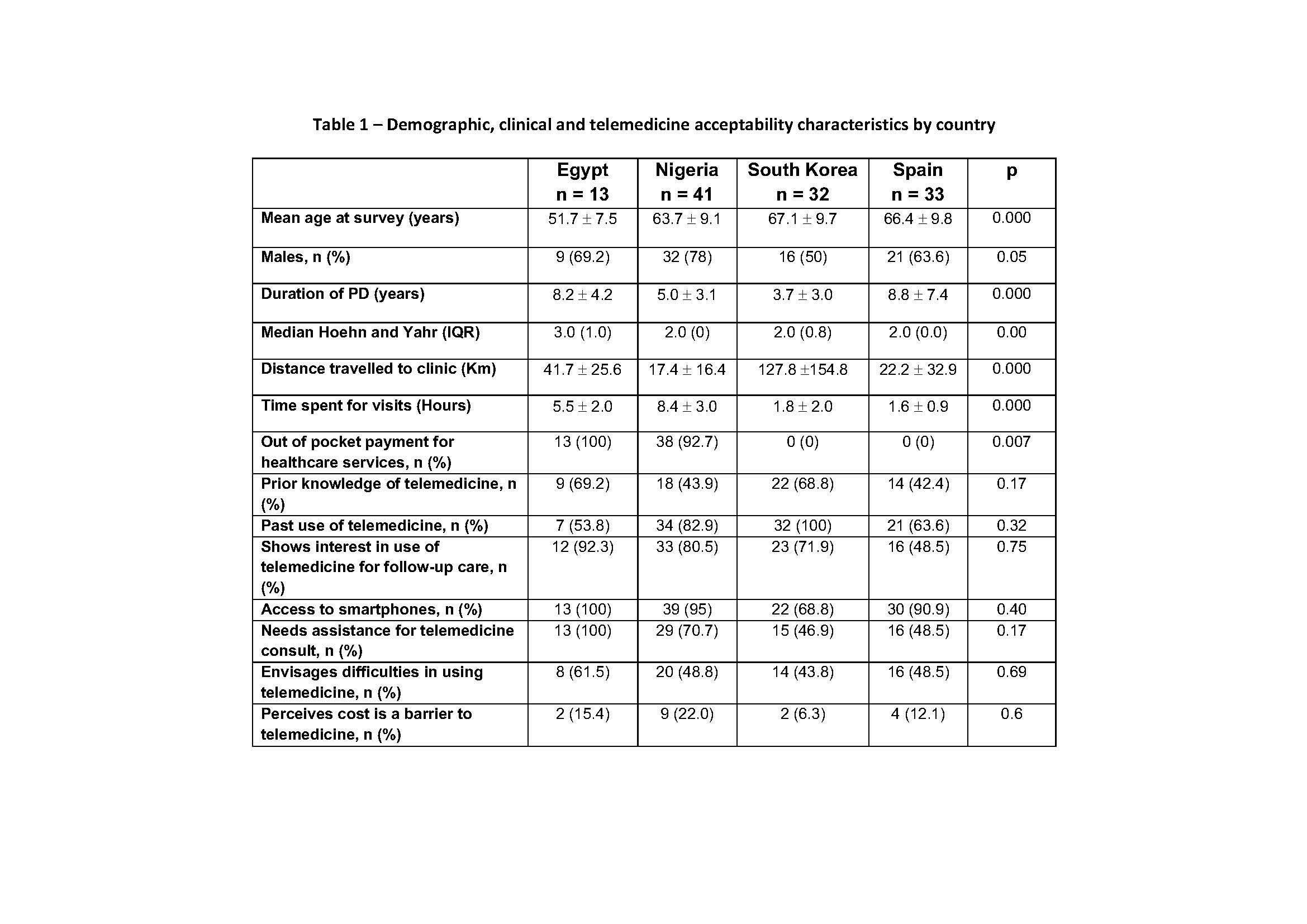
Results: Preliminary data are from 136 participants with parkinsonism, (PD of 119) from 4 countries: Egypt, Nigeria, South Korea and Spain. Mean age of PD was 63.4 ± 10.9 years, males 78 (65.5%), and median H and Y stage of 2 (IQR 0). PD distribution, clinical characteristics and telemedicine acceptability by country are displayed in Table 1. PD who were not interested in telemedicine were older (68.0 ± 63.1 versus 63.1 ±11.1 years; p = 0.03) and had fewer years of education (9.6 ± 4.1 versus 12.3 ± 4.6 years; p = 0.01).
Conclusion: Knowledge, interest, access, difficulties and barriers to telemedicine may be similar among countries despite differences in healthcare systems and PD characteristics
To cite this abstract in AMA style:
O. Ojo, JH. Ahn, Z. Aldaajani, J. Bajwa, A. Bustillo, A. Cardozo, M. Dekker, E. Eldayem, Z. Mari, A. Shalash, M. Shackleford, M. Spindler, J. Youn, E. Cubo, N. Okubadejo. An International Pre-Implementation Survey To Assess The Acceptability Of Telemedicine As An Alternative To In-Person Clinic Consultations For PD [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/an-international-pre-implementation-survey-to-assess-the-acceptability-of-telemedicine-as-an-alternative-to-in-person-clinic-consultations-for-pd/. Accessed April 3, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/an-international-pre-implementation-survey-to-assess-the-acceptability-of-telemedicine-as-an-alternative-to-in-person-clinic-consultations-for-pd/