Category: Other
Objective: Movement disorders in autoimmune encephalitis are common. The mainly differential in this case are epileptic movements, as the new onset status epilepticus (NOSE). An electroencephalogram (EEG) is the study of choice to differentiate both conditions; however, the interpretation’s variability could result in an erroneous diagnosis and therapeutic algorithm.
Background: Lingual myorrhythmia is a type of hyperkinetic movement disorder that belongs in the spectrum of orofacial dyskinesias and is a cause that mimics a NOSE. We report the case of a 49-years-old male patient with autoimmune encephalitis and facial dyskinesias.
Method: A previously healthy patient presented an acute psychotic episode and a non-epileptic movement disorder classified as orofacial dyskinesia initially classified as a NOSE. Due to high suspicion of an infectious central nervous system cause, a lumbar puncture was performed, revealing an inflammatory cerebrospinal fluid due to lymphocytic pleocytosis. Infectious etiologies were ruled out, and later, positive NMDA antibodies in cerebrospinal fluid were reported. The brain MRI scan was unremarkable. The final diagnosis was autoimmune encephalitis NMDA-mediated.
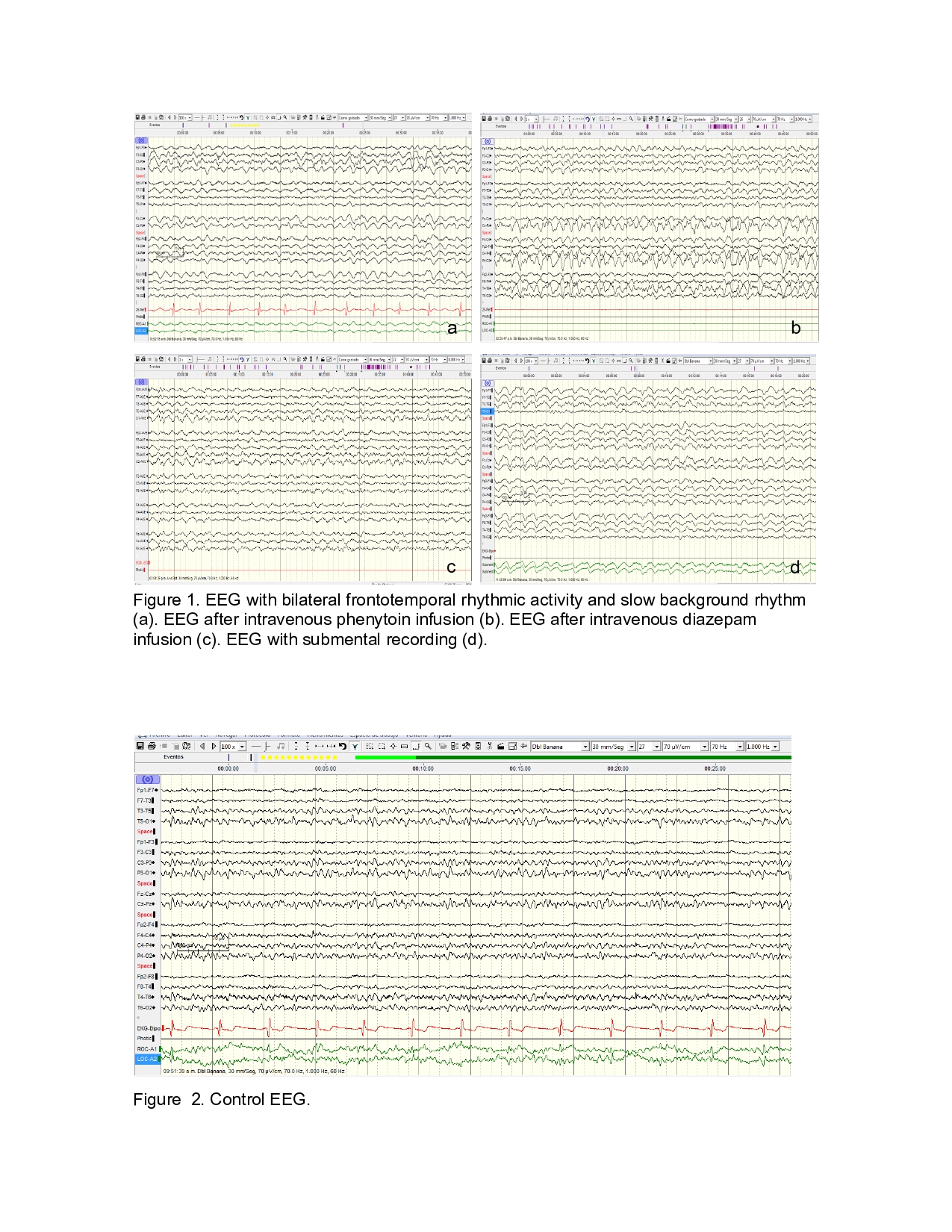
Results: Our diagnosis approach includes an electroencephalogram (EEG) during the phenomenon of lingual myorrhythmia that showed a continuous bilateral frontotemporal delta rhythmic activity with spatiotemporal evolution after intravenous administration of phenytoin and diazepam. Submental electrode placement showed a rhythmic and monomorphic artifact synchronized with the bilateral frontotemporal rhythmic delta activity. Thus, the suspicion of status epilepticus was dismissed. The patient presented clinical improvement after treatment with high-dose steroids, plasma exchange, and rituximab. With complete remission of electroencephalography findings.
Conclusion: The lingual myorrhythmia can mimic delta rhythmic activity in the EEG with slowing rhythm basal and simulate a status epilepticus. We suggested the use of submental electrodes to differentiate movement artifacts from epileptic activity.
References: 1. Midgley L, Kelleher E, Zandi MS. Autoimmune encephalitis. Br J Hosp Med (Lond) 2018 Sep 2;79(9):C134-C137. doi: 10.12968/hmed.2018.79.9.C134. 2. Gillinder L, Warren N, Hartel G, Dionisio S, O’Gorman C. EEG findings in NMDA encephalitis – A systematic review. Seizure 2019 Feb;65:20-24. doi: 10.1016/j.seizure.2018.12.015. 3. Kaplan PW, Probasco J. Limbic and new-onset refractory tonic status epilepticus (NORSE) in anti-NMDAR encephalitis. Clin Neurophysiol Pract 2017 Jul 1;2:140-143. DOI: 10.1016/j.cnp.2017.06.003. 4. Kim H, Ryu H, Kang JK. Anti-NMDA Receptor Antibody Encephalitis Presenting with Unilateral Non-convulsive Status Epilepticus in a Male Patient. J Epilepsy Res 2015 Jun 30;5(1):17-9. DOI: 10.14581/jer.15004.
To cite this abstract in AMA style:
J. Diestel Bautista, Z. Rojas Cheje, A. Michel Chavez, C. Mendoza Tejeda, D. Rebolledo García, H. Sentíes Madrid. Facial dyskinesias mimics a new-onset status epilepticus in a patient with autoimmune encephalitis [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/facial-dyskinesias-mimics-a-new-onset-status-epilepticus-in-a-patient-with-autoimmune-encephalitis/. Accessed December 27, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/facial-dyskinesias-mimics-a-new-onset-status-epilepticus-in-a-patient-with-autoimmune-encephalitis/