Objective: The aim of this study was to assess Parkinson’s disease (PD) patients’ preferences on how to take medical decisions.
Background: Patients’ decisions are mainly based on evidence, professionals counselling and the individual preference [1]. The ladder remains a personal perspective, which needs to be taken into account in the clinician‘s interview. Shared decision-making (SDM) can guide patients in their health care decisions to prevent potential discontinuation of adherence [2]. Current conversation strategies should be revised by emphasizing the consequences of SDM on healthcare and health outcome [3]. Advanced PD patients wish to be involved in the medical decision-making [4]. However, the impact of patients’ characteristics on their preferred decision type are not yet fully understood.
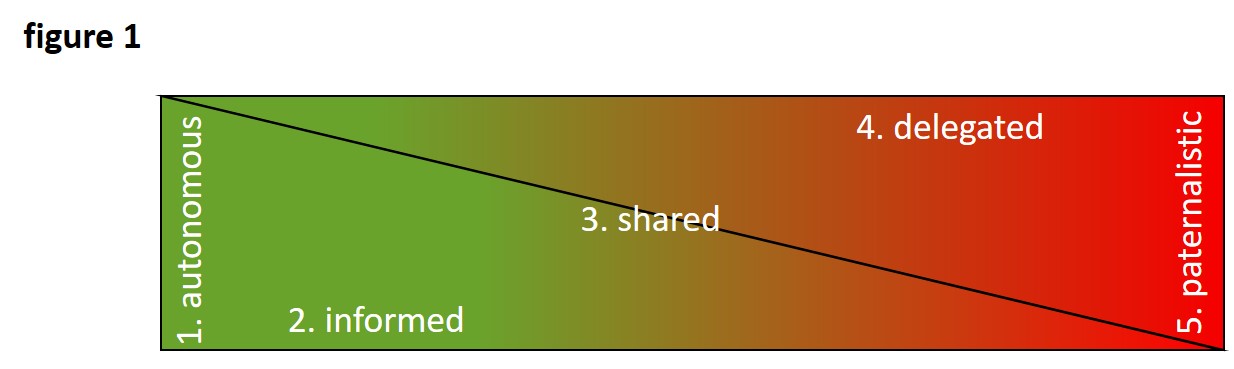
Method: We asked 232 PD patients (33-86 years old, mean age 65 years, 58% men) in a personal, structured interview about their preferential way to take medical decisions. They could choose between 5 different categories (“autonomous”, “informed”, “shared”, “delegated”, “paternalistic”), which were described both by text and picture (figure 1) [5]. In addition, patients’ characteristics (gender, school education, relationship) were recorded. Descriptive statistics were performed by SPSS software, version 26.
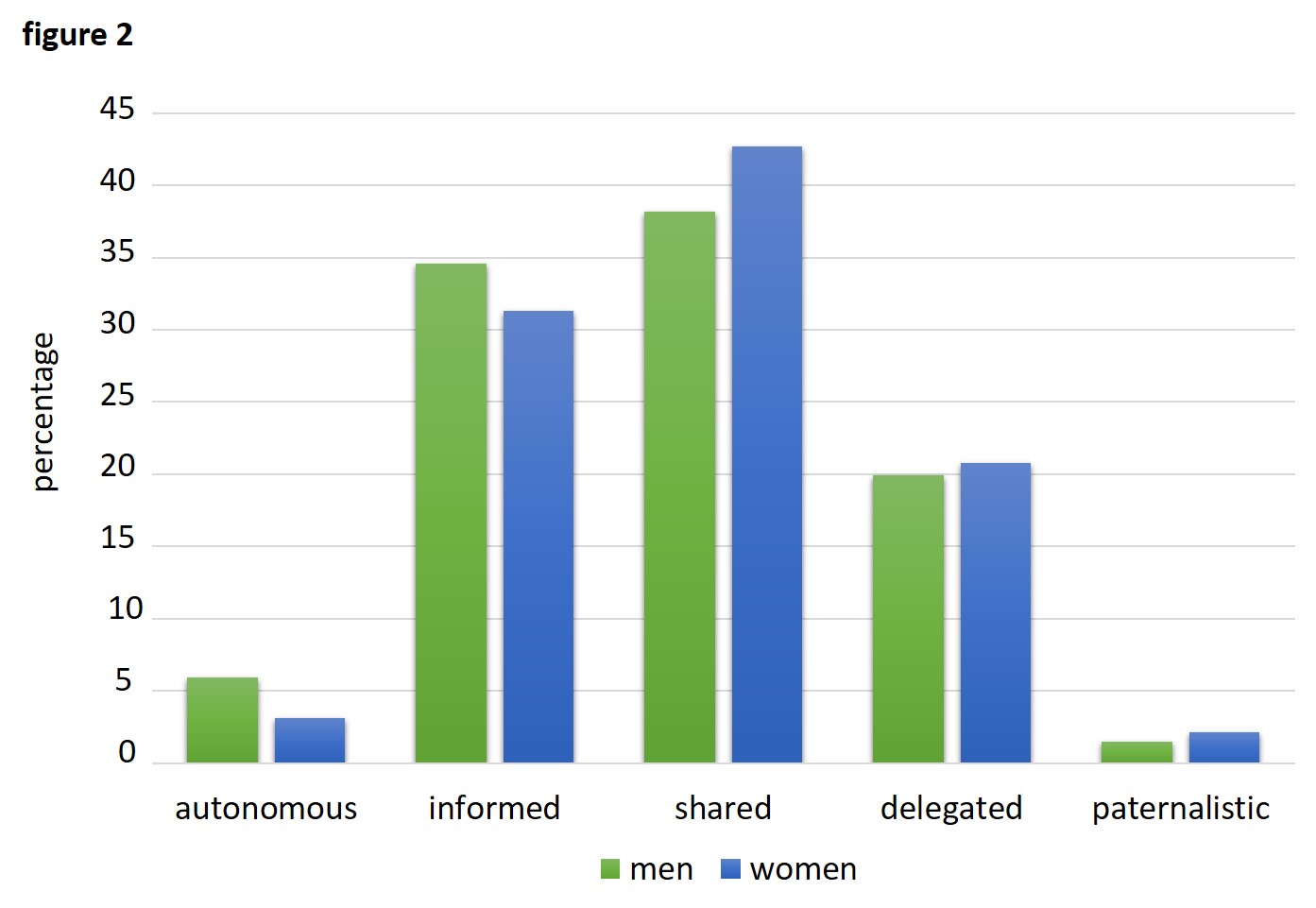
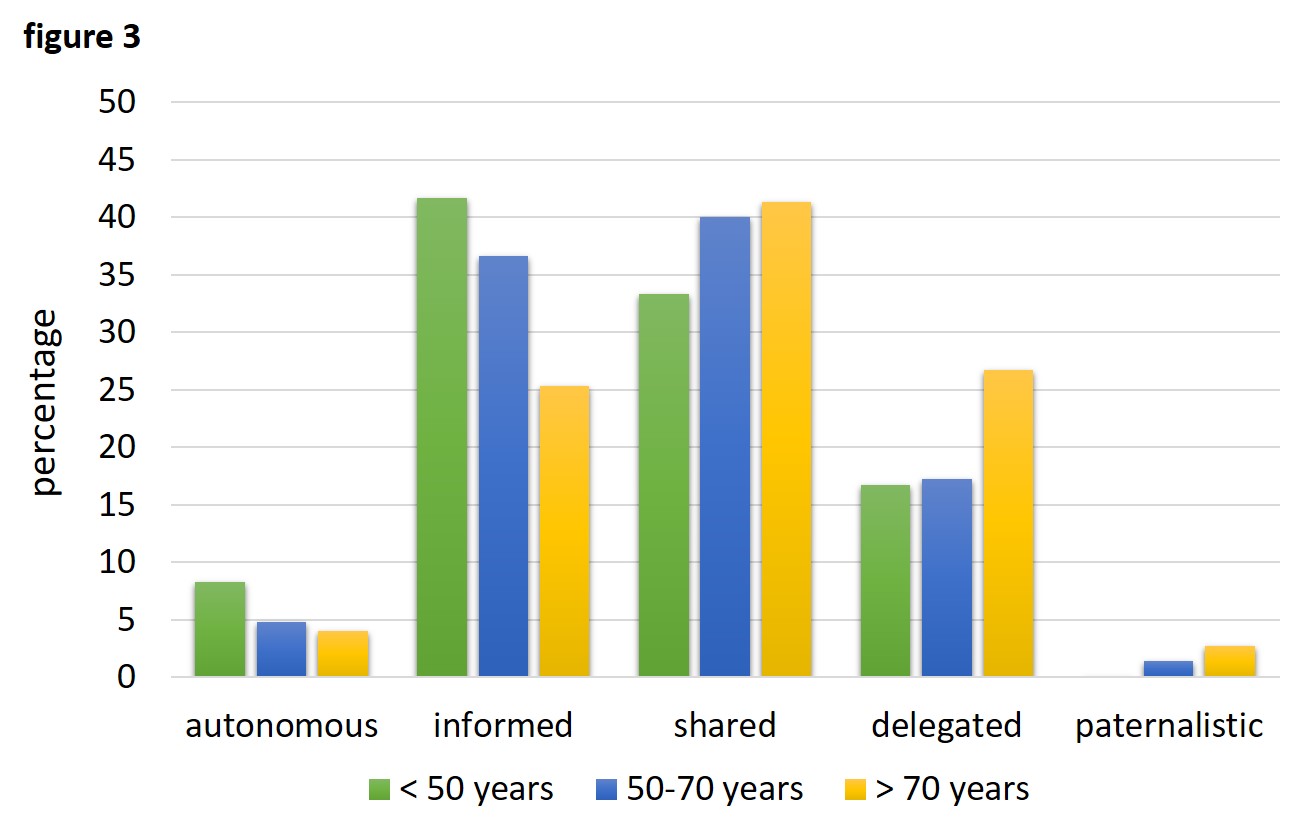
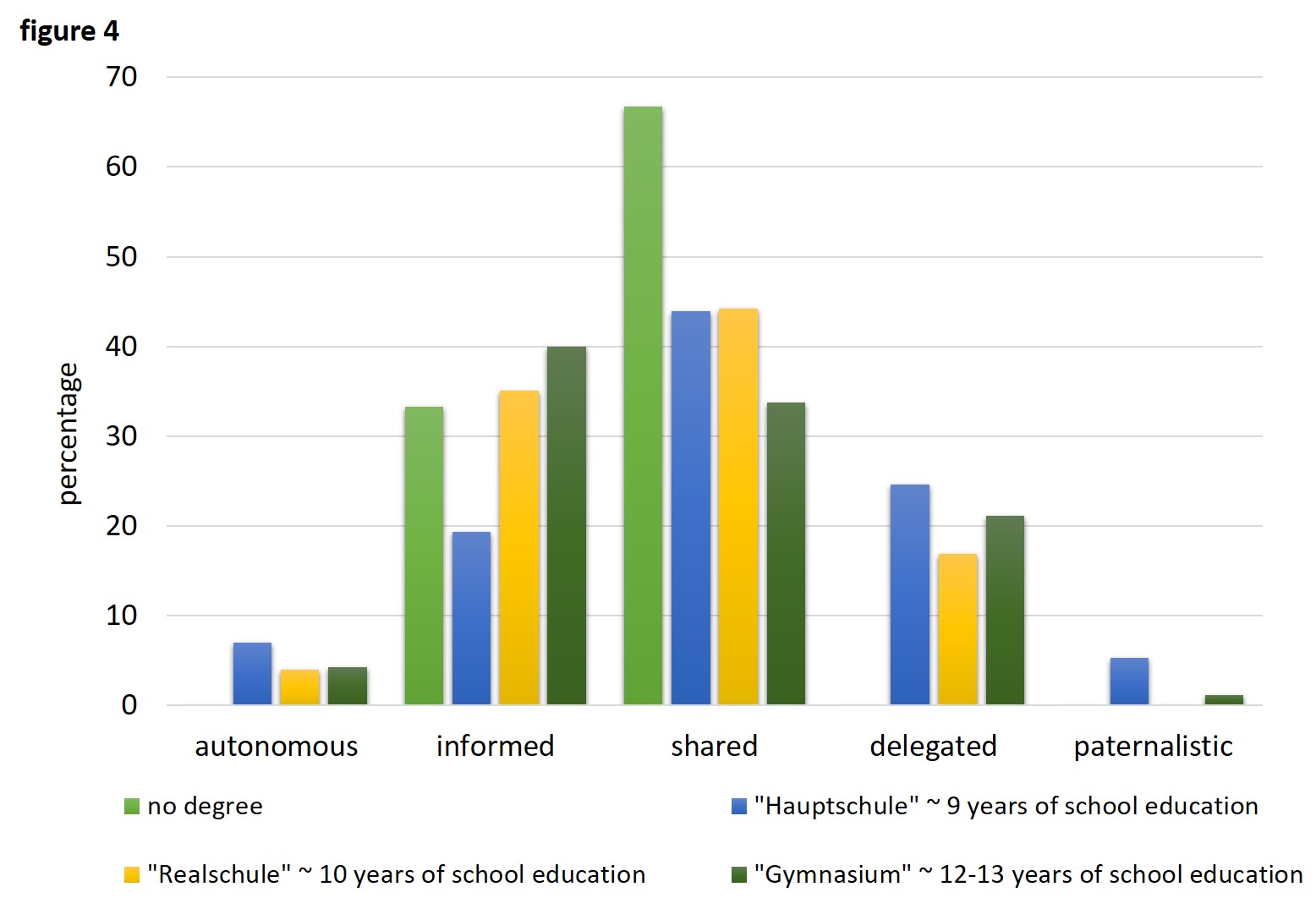
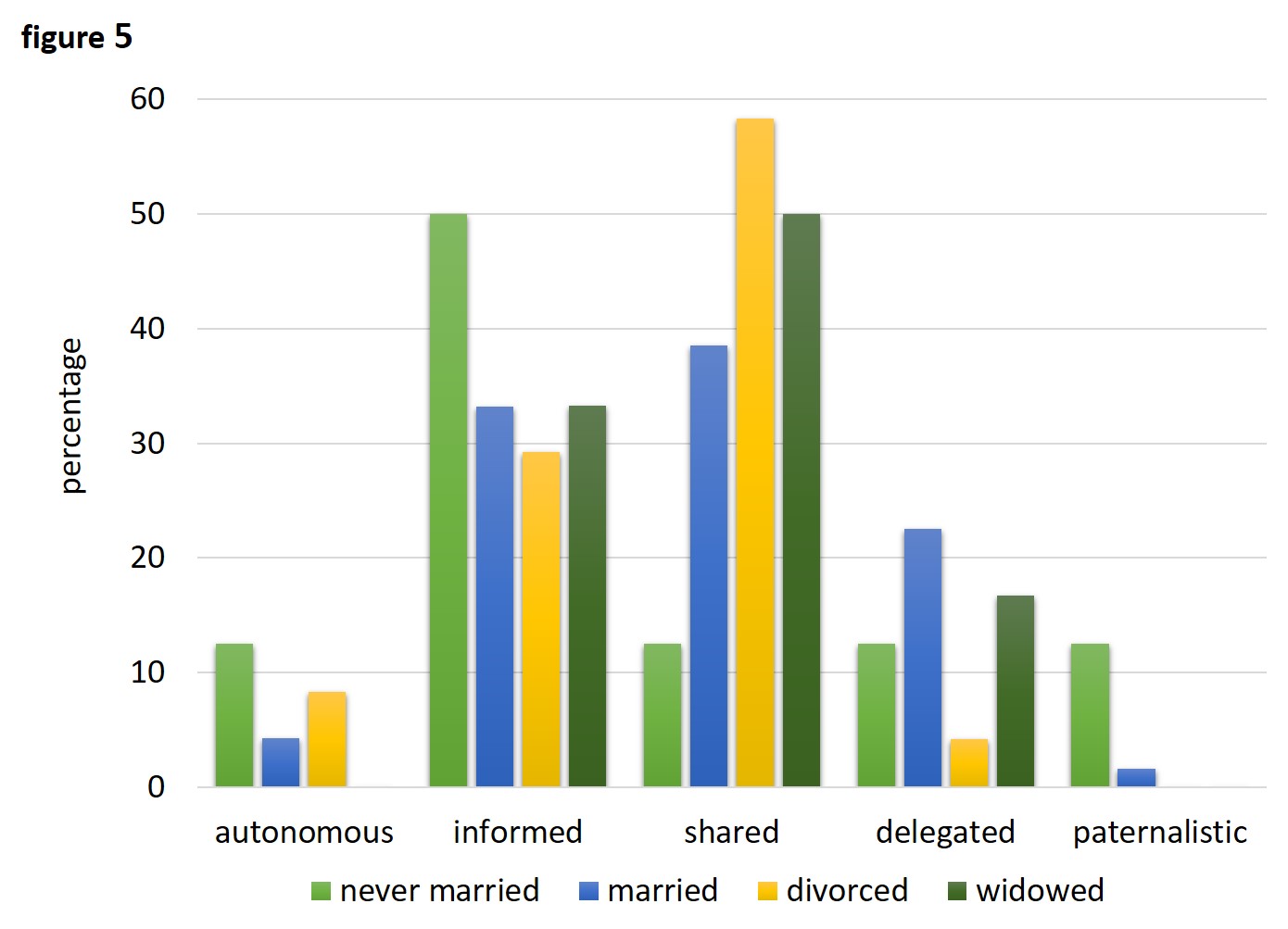
Results: Both women and men wished to share their decisions with the clinician in charge (figure 2). Patients younger than 50 years (n=12) chose an “informed” consent with a more autonomous decision-making compared to older patients (>70 years) (n=75), which tended to favour a more “delegated” decision (figure 3). A “shared” approach is the preferential type for patients with no educational degree (n=3) and for those with 9-10 years of school education (n=134). There is a slight preference towards an “informed” consent in patients finishing 12-13 years of school with a graduate degree (n=95) (figure 4). In the group of patients never being married (n=8), an “informed” consent is preferred over a “shared” decision. Married patients (n=187) favour a “shared” decision as well as divorced (n=24) and widowed (n=12) patients (figure 5). In summary, a “shared” decision-making approach is the most favourable decision-making type in PD.
Conclusion: Our findings describe PD patients’ preferences on medical decision-making. These insights might help to improve the physician´s ability of counselling for optimized future patients’ therapy adherence.
References: 1. van den Heuvel, L., et al., Quadruple Decision Making for Parkinson’s Disease Patients: Combining Expert Opinion, Patient Preferences, Scientific Evidence, and Big Data Approaches to Reach Precision Medicine. J Parkinsons Dis, 2020. 10(1): p. 223-231. 2. Gustin, A.N., Jr., Shared Decision-Making. Anesthesiol Clin, 2019. 37(3): p. 573-580. 3. Elwyn, G., D.L. Frosch, and S. Kobrin, Implementing shared decision-making: consider all the consequences. Implement Sci, 2016. 11: p. 114. 4. Nijhuis, F.A.P., et al., The Patient’s Perspective on Shared Decision-Making in Advanced Parkinson’s Disease: A Cross-Sectional Survey Study. Front Neurol, 2019. 10: p. 896. 5. Solari, A., et al., Role Preferences of People with Multiple Sclerosis: Image-Revised, Computerized Self-Administered Version of the Control Preference Scale. PLoS One, 2013. 8(6): p. e66127.
To cite this abstract in AMA style:
E. Gülke, C. Wargel, A. Rahn, A. Solari, C. Buhmann, C. Gerloff, C. Heesen, M. Pötter-Nerger. Patients’ perspectives on shared decision-making in Parkinson´s disease [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/patients-perspectives-on-shared-decision-making-in-parkinsons-disease/. Accessed April 2, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/patients-perspectives-on-shared-decision-making-in-parkinsons-disease/