Objective: The goal of this study is to describe the factors that may have an impact on Continuous Subcutaneous Apomorphine Infusion (CSAI) therapy initiation and to describe any link between treatments combination and the patient’s profile.
Background: CSAI is one solution for advanced Parkinson’s disease (PD) patients to avoid fluctuations [1]. An adequate balance between oral levodopa treatment and CSAI is usually sought for weeks requiring multiple hospitalisations and outpatients visits. In a context in which no official guidelines have been published about care organisation of PD patients with CSAI therapy, there is a lack of knowledge regarding proceedings of follow-up to ensure the efficiency of health expenditure.
Method: We used data from a single center of the OPTIPUMP cohort study (Pitié-Salpêtrière Hospital) which was a prospective, open-label, observational, multicenter study. Treatments and PD scorings were reviewed during hospitalisation as part of the follow-up of patients after CSAI therapy initiation.
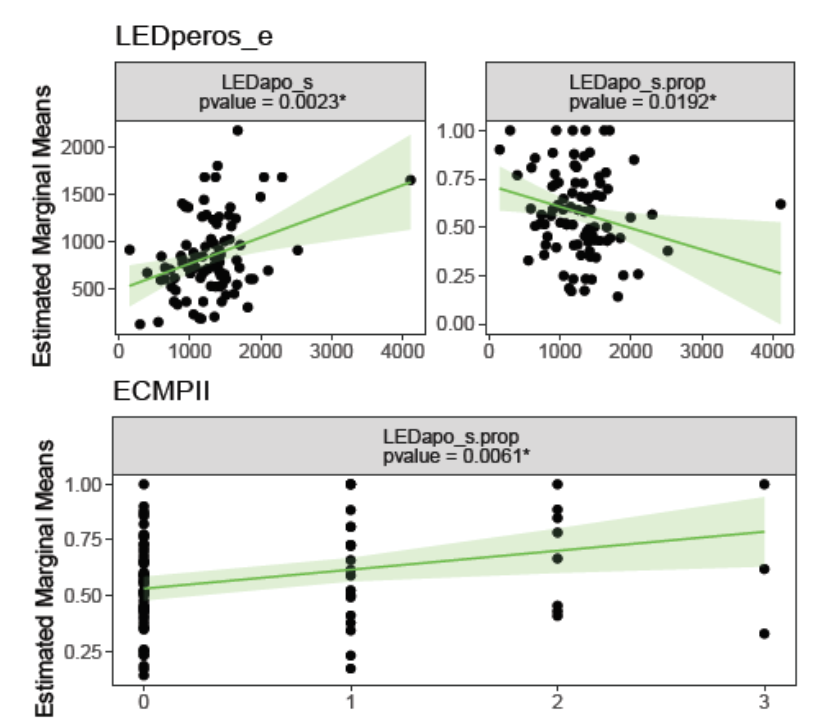
We modeled levodopa Equivalent Doses (LED) of oral treatment and of apomorphine and the ratio of apomorphine LED compared to total LED at initiation of CSAI therapy depending on disease assessment (standard PD scales).
Results: 89 PD patients programmed for CSAI therapy (47 women; median age= 64) were included. Mean duration of the disease is 11 years.
Statistical models show significant effects of:
– Oral treatment LED on apomorphine LED (p value= 0,0023)
– Oral treatment LED on the proportion of apomorphine LED (p value= 0,0192)
– Part 2 of the behavioral assessment in PD scale on the proportion of apomorphine LED (p value= 0,0061)
Conclusion: The results suggest that:
– the more the oral antiparkinsonian treatment, the more the apomorphine amount prescribed at initiation, which seems coherent with the total amount of treatment given to patients
– the proportion of apomorphine is higher when the oral LED is low
– when apathy is more pronounced, the apomorphine in the total antiparkinsonian treatment is predominant.
Those results are a first insight on the organization of care for advanced PD patients with CSAI therapy. They may trigger new thinking during the process of pump initiation.
This work will be completed by the analysis of the evolution of CSAI therapy during 2 years according to PD symptoms progress; work that will be available at the time of MDS congress.
References: [1] Melamed, E., Ziv, I., & Djaldetti, R. (2007). Management of motor complications in advanced Parkinson’s disease. Movement disorders: official journal of the Movement Disorder Society, 22(S17), S379-S384.
To cite this abstract in AMA style:
C. Virbel-Fleischman, M. Houot, Y. Rétory, S. Hardy, J.C Corvol, D. Grabli. A monocentric experience of Apomorphine pump follow-up on PD patients: The Optipump Cohort [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/a-monocentric-experience-of-apomorphine-pump-follow-up-on-pd-patients-the-optipump-cohort/. Accessed April 1, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/a-monocentric-experience-of-apomorphine-pump-follow-up-on-pd-patients-the-optipump-cohort/