Objective: To investigate possible differences in phenomenology and temporal profile of dyskinesias in patients with Parkinson’s disease (PD) after challenge doses with levodopa alone or levodopa in combination with ropinirole.
Background: Dyskinesias are a common problem in PD patients with a long duration of disease and treatment, and their pathophysiology involves multiple neuronal circuits that are regulated by different types of dopamine receptors. While levodopa stimulates both D1 and D2-family dopamine receptors, ropinirole has selective affinity for the D2 class (particularly D2-D3) and has, in addition, a longer half-life than levodopa.
Method: 12 patients with PD and a history of dyskinesias or dystonias where included in the study. Patients received challenge tests on two occasions using either levodopa alone (150% of usual morning dose) or a combination of levodopa and ropinirole with equal levodopa-equivalent doses. The challenge tests were performed after pausing all antiparkinsonian agents for one day, with amantadine being paused 1 week prior to the first challenge test. All patients received both challenge tests in a random order and within 2 weeks. Dyskinesias were rated prior and every 30 minutes after challenge drug dosing for a total of 300 minutes using the Clinical Dyskinesia Rating Scale (CDRS), which yields separate ratings of hyperkinesia and dystonia in different body parts.
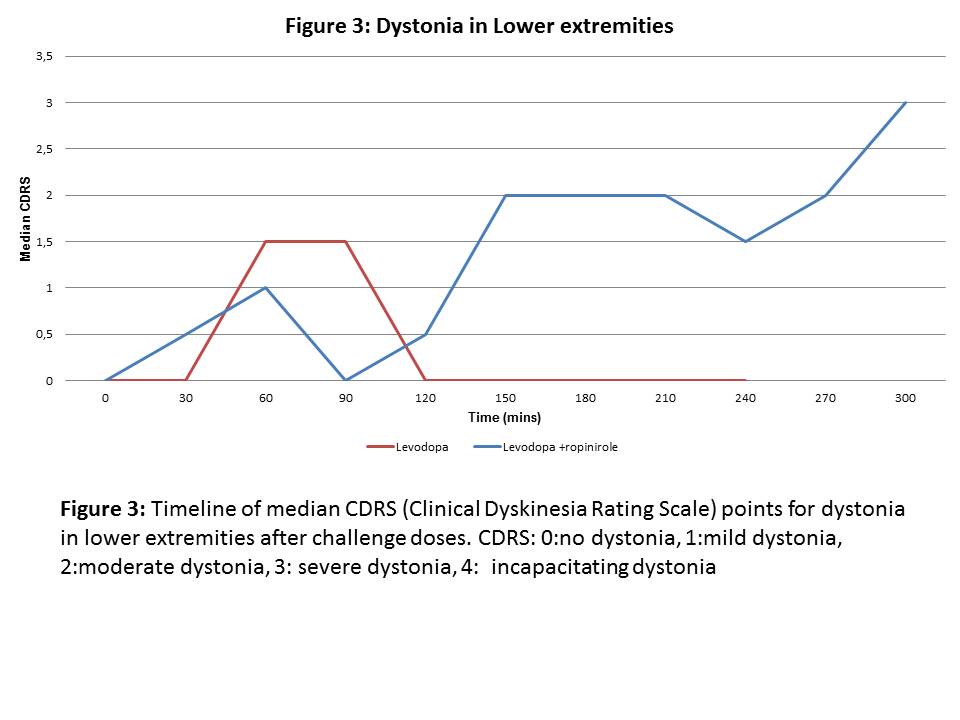
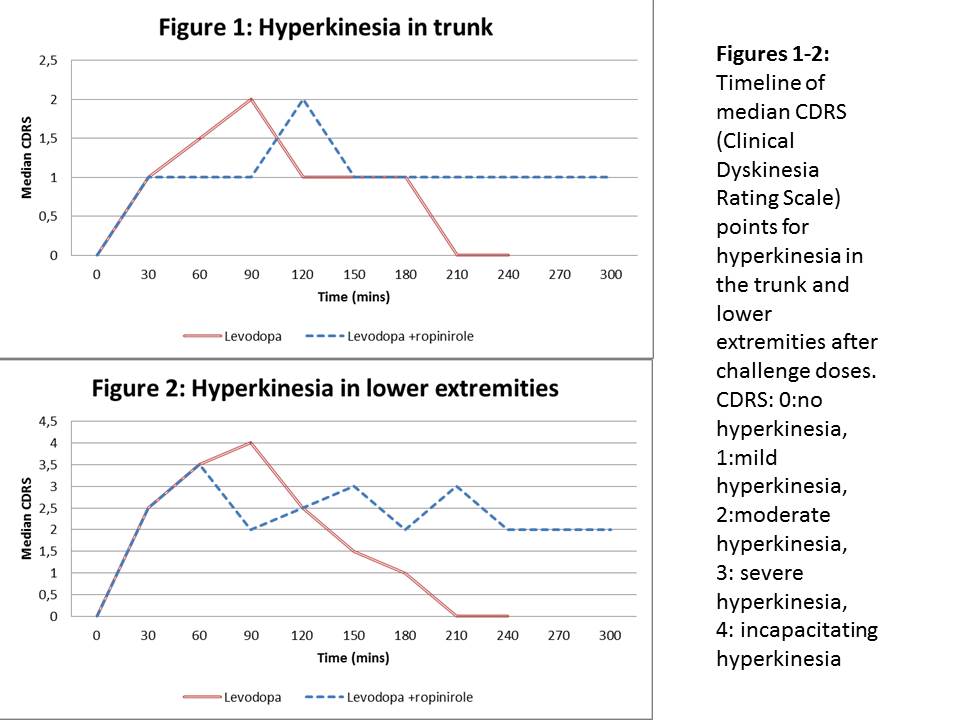
Results: All patients experienced dyskinesias following both challenge tests. The medication effect and the duration of dyskinesias were longer after the challenge dose containing levodopa and ropinirole. We detected a significantly higher hyperkinesia score following administration of levodopa and ropinirole in the trunk and in lower extremities at 210 minutes (figures 1-2), as well as a significantly higher dystonia score in the lower extremities at 180 and 210 minutes after the challenge dose (figure 3).
Conclusion: When ropinirole is added to the dopaminergic medications, maintaining the same levodopa-equivalent dose, hyperkinesias are experienced for a longer time period and dystonias appear in the late phase of the dose-response time curve. This suggests that dystonias become more prominent when the effect of levodopa stimulation subsides and the D2/3 receptor stimulation by ropinirole persists. These observations will be verified in additional patients.
References: [1] Tran TN, Vo TNN, Frei K, Truong DD. Levodopa-induced dyskinesia: clinical features, incidence, and risk factors. Journal of Neural Transmission. 2018;125(8):1109-17. [2] Cenci MA, Jorntell H, Petersson P. On the neuronal circuitry mediating LDOPA-induced dyskinesia. J Neural Transm (Vienna). 2018;125(8):1157-69. [3] Hagell P, Widner H. Clinical rating of dyskinesias in Parkinson’s disease: use and reliability of a new rating scale. Mov Disord. 1999;14(3):448-55.
To cite this abstract in AMA style:
S. Grigoriou, S. Christiansson, P. Odin, M.A Cenci. Impact of dopamine 2/3 receptor agonists on the phenomenology of L-DOPA-induced dyskinesia in patients with Parkinson’s disease [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/impact-of-dopamine-2-3-receptor-agonists-on-the-phenomenology-of-l-dopa-induced-dyskinesia-in-patients-with-parkinsons-disease/. Accessed December 28, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/impact-of-dopamine-2-3-receptor-agonists-on-the-phenomenology-of-l-dopa-induced-dyskinesia-in-patients-with-parkinsons-disease/