Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To assess the effects of co-morbidities on sleep patterns in PD.
Background: Parkinson’s disease is a progressive neurodegenerative disease. The non-motor symptoms are said to be more disabling than the motor feature, sleep disorders are found in 98% of PD patients, they may result from the disease process, medications or nocturnal disturbances. PD could have hypertension, diabetes, obesity as co-morbidities. The relationship of sleep disorders and some morbidities has been reported to be bidirectional.
The study seeks to find out if the presence of co-morbidities in PD changes the sleep disorders patterns.
Method: This was a descriptive cross-sectional study conducted at the University College Hospital, Ibadan. Eighty- four consecutive consenting adults with PD were recruited. Patient’s information including socio-demographic data, medical and social history, sleep hygiene, PD history and medications were recorded.
PD patients were diagnosed according to specified diagnostic criteria and rating scales of PD staging (Hoehn &Yahr), cognitive functioning (Mini Mental State Examination (MMSE), sleep disorders (Parkinson’s disease sleep scale (PDSS), Epworth Sleepiness Scale(ESS), REM behavioural disorder (REMBD) screening questionnaire, STOP BANG for Obstructive sleep apneas (OSA)and quality of life (PD Quality of Life Questionnaire(PDQOL-39) were applied on all PD patients. Statistical significance was set at p<0.05.
Results: Eighty-four (84) PD patients were recruited. The mean age of PD participants was-70.5 (SD-8.8) years. They included 55(65.5%) males and 29 (34.5%) females. Hypertension was the predominant co-morbidity of about 49 (58.3%) in PD participants and diabetes was diagnosed in 14 (16.7%) in PD participants.
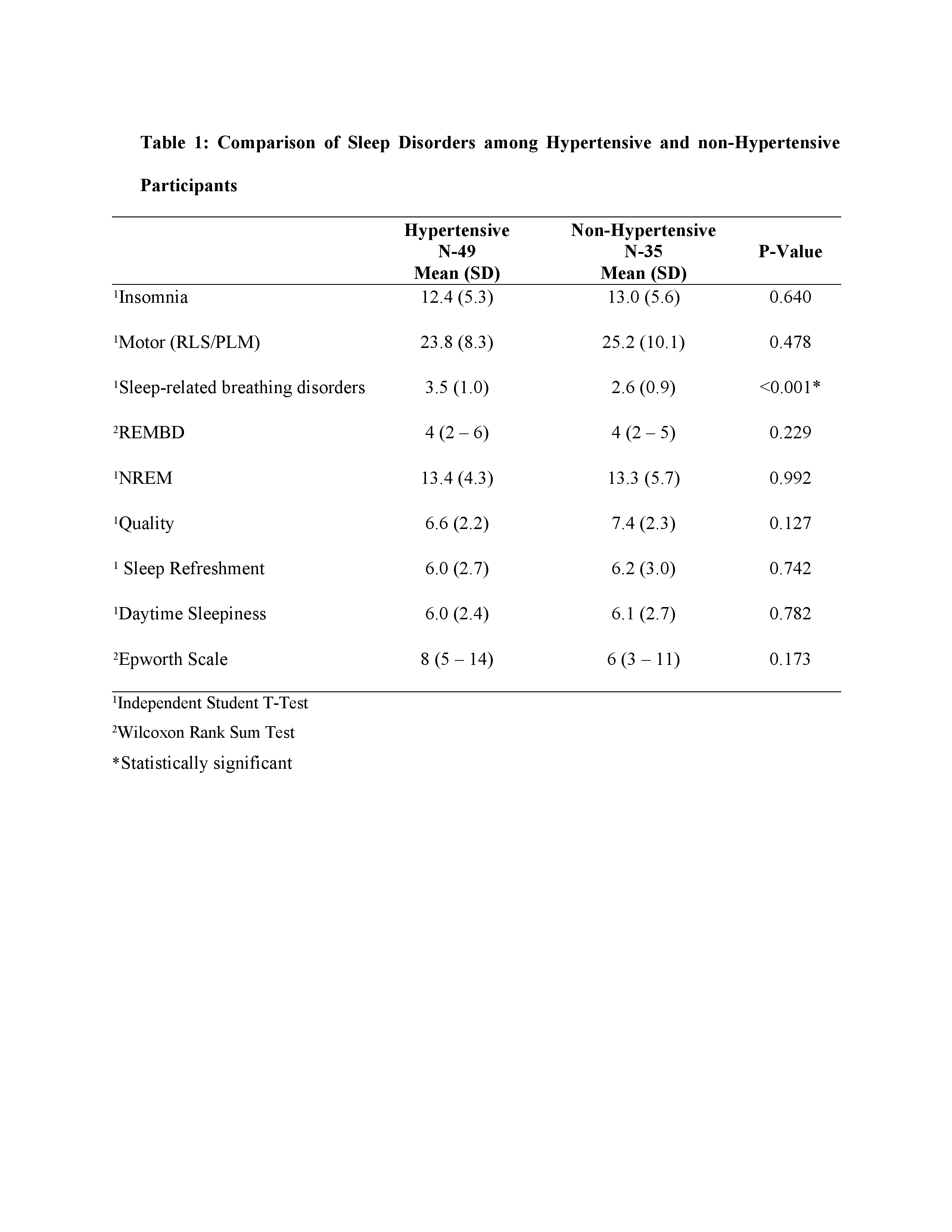
Sleep- related breathing disorders attained statistical significance between the PD hypertensive sub-group 3.5(SD-1.0) versus PD non- hypertensive sub-group 2.6(SD-0.9) with a p- value of <.001.
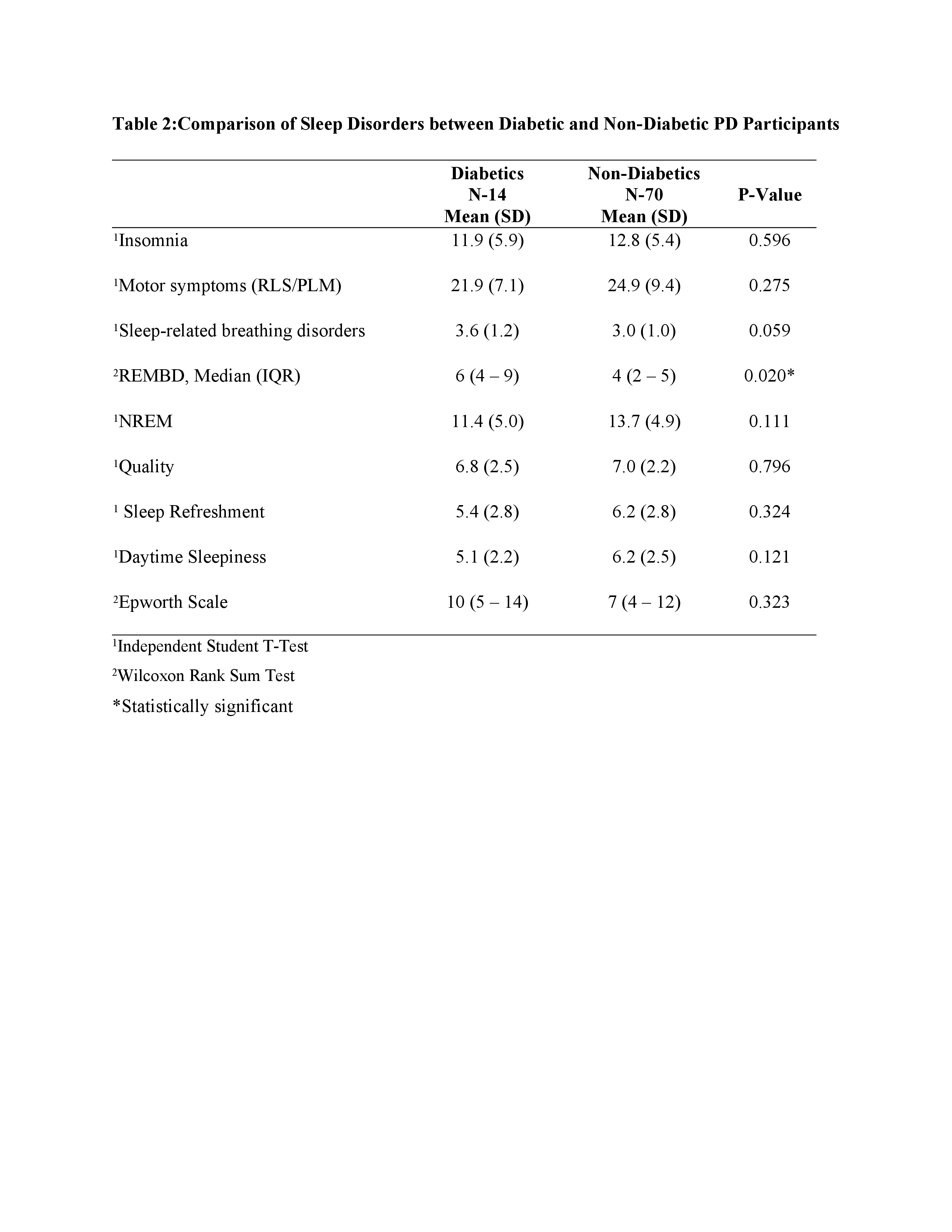
Among PD participants with diabetes and those without, REMBD attained statistically significant value with median score of in 6(IQR 4-9) in the diabetic and 4(IQR 2-5) in non-diabetic with a p-value of 0.020.
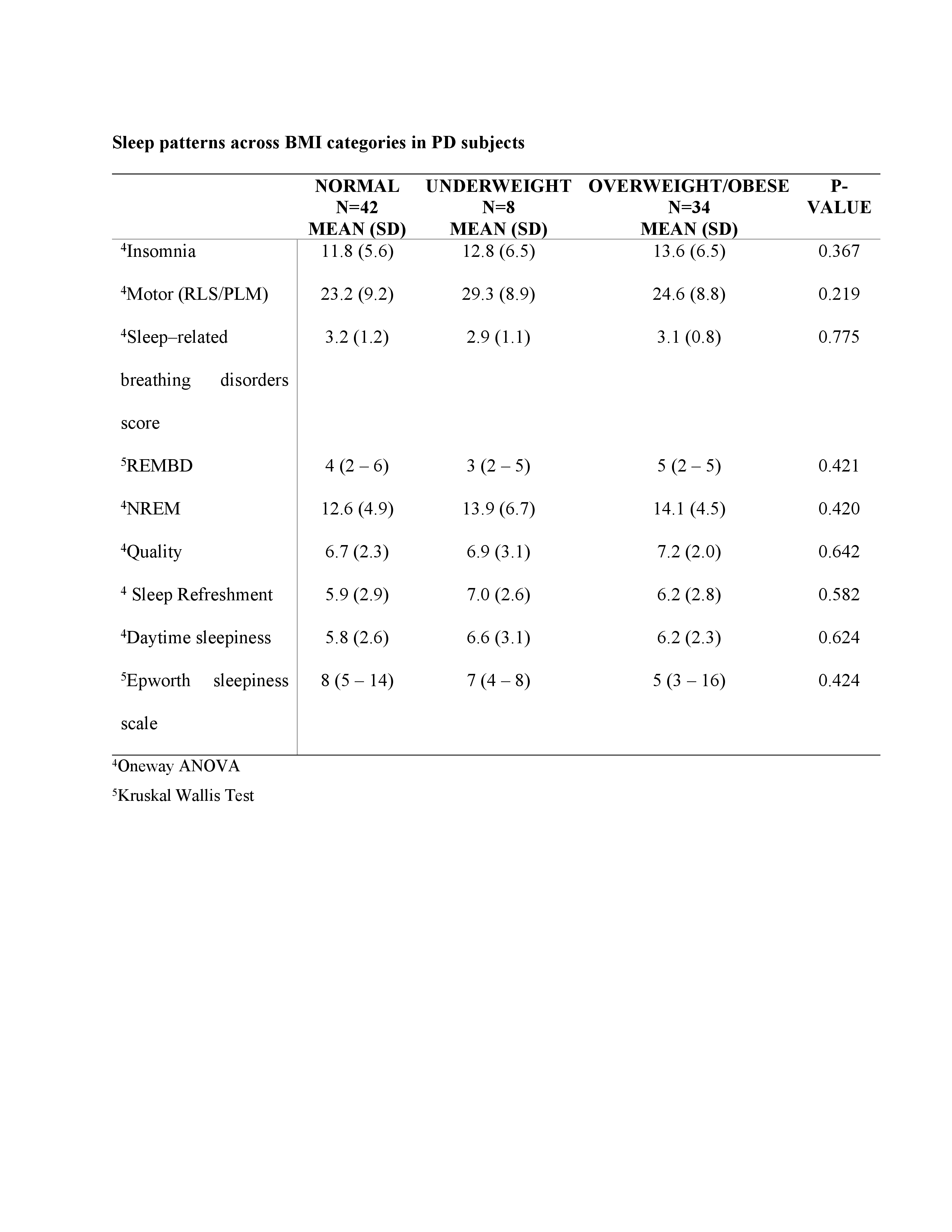
There were no statistically significant differences in the sleep disorders across all the different BMI categories both the PD subjects and controls.
Conclusion: Some sleep disorders are more prevalent when PD coexist with comorbidities and this should be borne in mind in the management of PD patients.
To cite this abstract in AMA style:
R. Oguntoye. Effects of Co-Morbidities on Sleep Patterns in Parkinson’s Disease: A Study of 84 Ibadan Patients [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/effects-of-co-morbidities-on-sleep-patterns-in-parkinsons-disease-a-study-of-84-ibadan-patients/. Accessed April 2, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/effects-of-co-morbidities-on-sleep-patterns-in-parkinsons-disease-a-study-of-84-ibadan-patients/