Category: Parkinson's Disease: Non-Motor Symptoms
Objective: The objects of the research were to investigate the clinical heterogeneity of orthostatic hypotension(OH) in PD Patients, to explore the possible risk factors for OH in PD patients and to improve medical diagnosis and treatment standard of OH.
Background: Autonomic dysfunction is a quite common non-motor symptom in PD patients and sometimes it may happen before motor symptoms, meanwhile OH is one of the most important clinical signs in autonomic nerve dysfunction.
Method: 150 patients with PD were enrolled in the Department of Neurology, Qilu Hospital of Shandong University, from January 2016 to March 2018. Blood pressure of patients were measured in supine position and in standing position after 1 minute, 3 minutes and 5 minutes. All patients during the ”on” period were assessed by the MDS-UDPRS I-IV, SCOPU-AUT, RBDSQ, OHQ-I and MMSE. The results were analyzed by Mann-Whitney U, Fisher’s Exact and the Logistic regression analysis. The decision tree model was used to furture analyze the data. All data were analyzed by R(3.33) software. Statistical significance was set at P0.05.
Results: 1.46 PD patients reached the OH criterion and the incidence of OH was 31%.
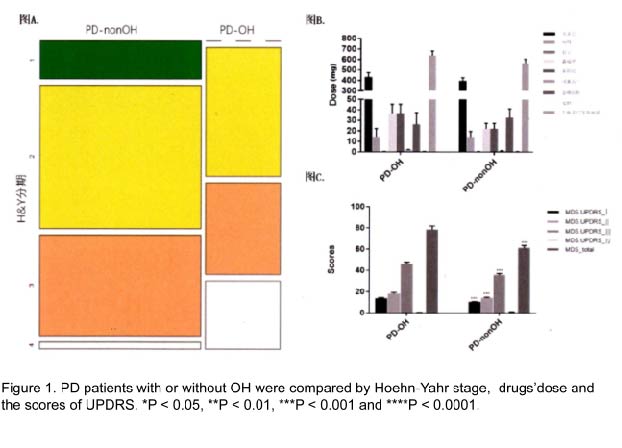
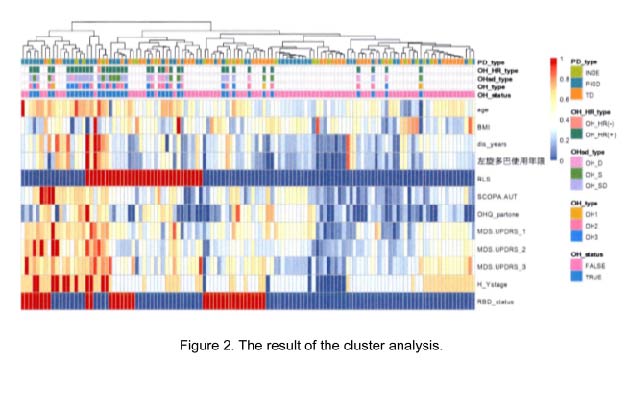
2. Single factor analysis and the cluster analysis both verified that there were significant differences between the two group-with and without OH in age, BMI, duration, Hoehn-Yahr stage, RBD, RLS, UPDRS I-III, SCOPA-AUT and OHQ-I.
3. Logistic regression analysis showed that low BMI, RLS, RBD scores or/and high UPDRS-I,OHQ-I scores were risk factors for OH.
4. The decision tree model showed that when the course of disease was longer than 5.1 years, there were 25 of the 48 PD patients developed OH, while BMl was less than 20.1, 23 of the 34 PD patients developed OH. Further, when UPDRS-I scores of those patients was greater than 12, there were 90% PD patients with OH. The accuracy of this model is 0.82, with the specificity 0.96 and the sensitivity 0.48.
Conclusion: 1.The incidence of OH in Parkinson’s disease was 31% in this study.
2.Compared PD patients without OH, those with OH were older, lower BMI, more advanced Hoehn&Yahr stage, a longer duration or high scores of SCOPA-AUT/MDS-UPDRS.
3.The scores of BMI, RLS, RBD, OHQ-I and UPDRS-I could better explain the occurrence of OH.
4.PD patients who courses of disease are longer than 5.1 years, BMI is less than 20.1 and the UPDRS-I scores are more than 12 were more likely to have OH.
To cite this abstract in AMA style:
P.Z Li, LL. Peng, J.L Wang, Y.M Liu. The Clinical Heterogeneity of Orthostatic Hypotension in PD Patients [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/the-clinical-heterogeneity-of-orthostatic-hypotension-in-pd-patients/. Accessed February 18, 2026.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-clinical-heterogeneity-of-orthostatic-hypotension-in-pd-patients/