Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To investigate Orthostatic hypotension (OH) feature in early onset Parkinson’s disease (EOPD) , especially delayed OH and acute OH post drug. To explore OH influence in motor function and non-motor function performance in EOPD, and its risk factors.
Background: Compared to late onset typical PD, EOPD are reported to have a more benign progression of disease, longer survival, lower score of autonomic dysfunction, less probability of dementia and gait disorders, and less non-motor symptoms. But knowledge of OH feature in EOPD was limited.
Method:
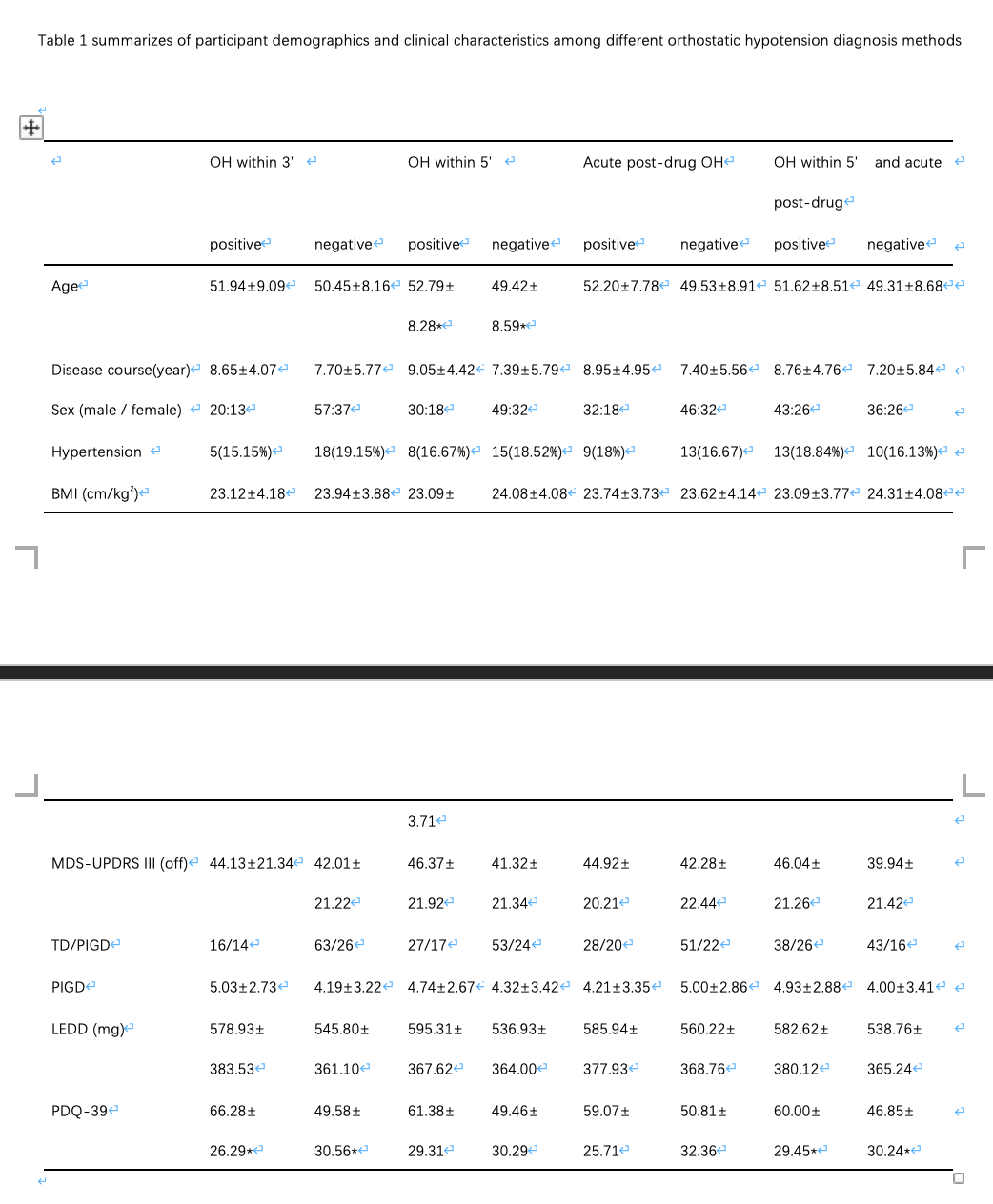
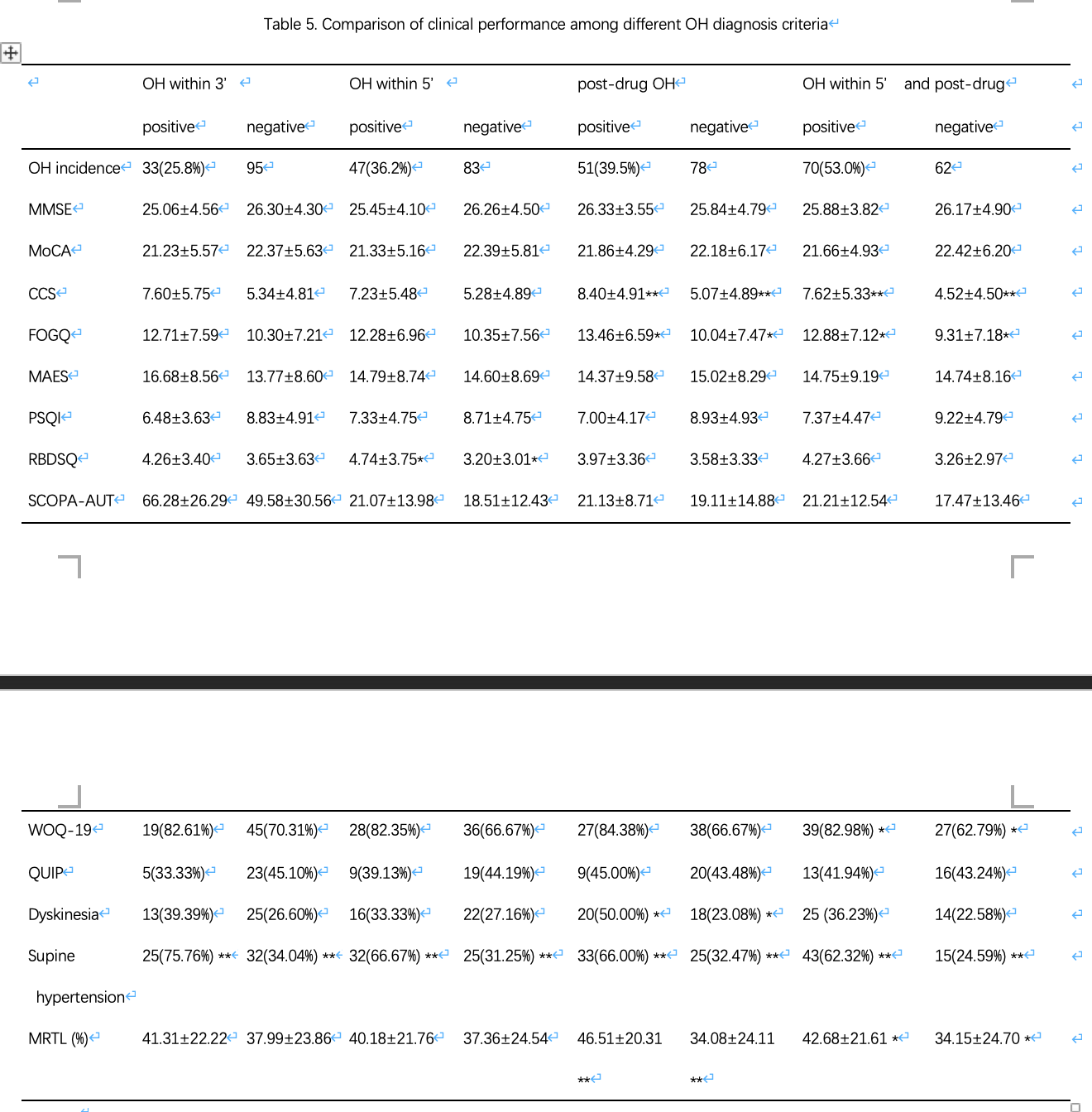
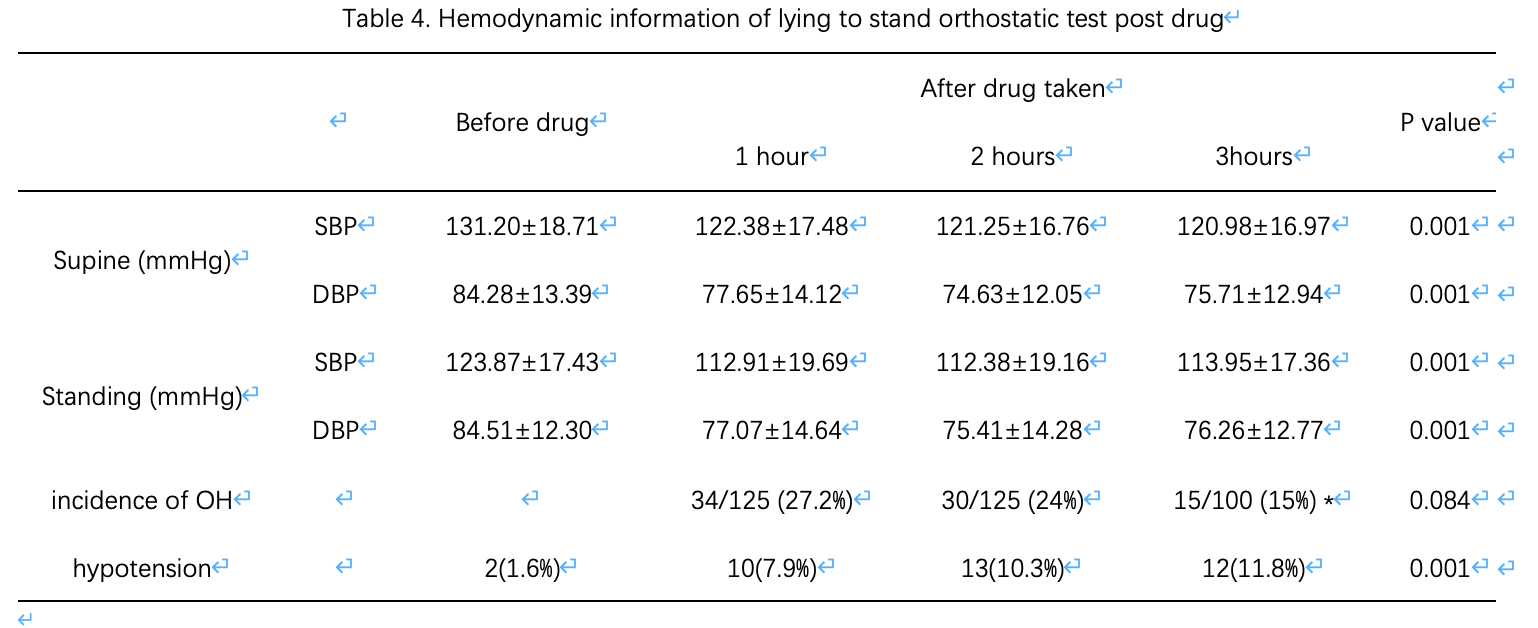
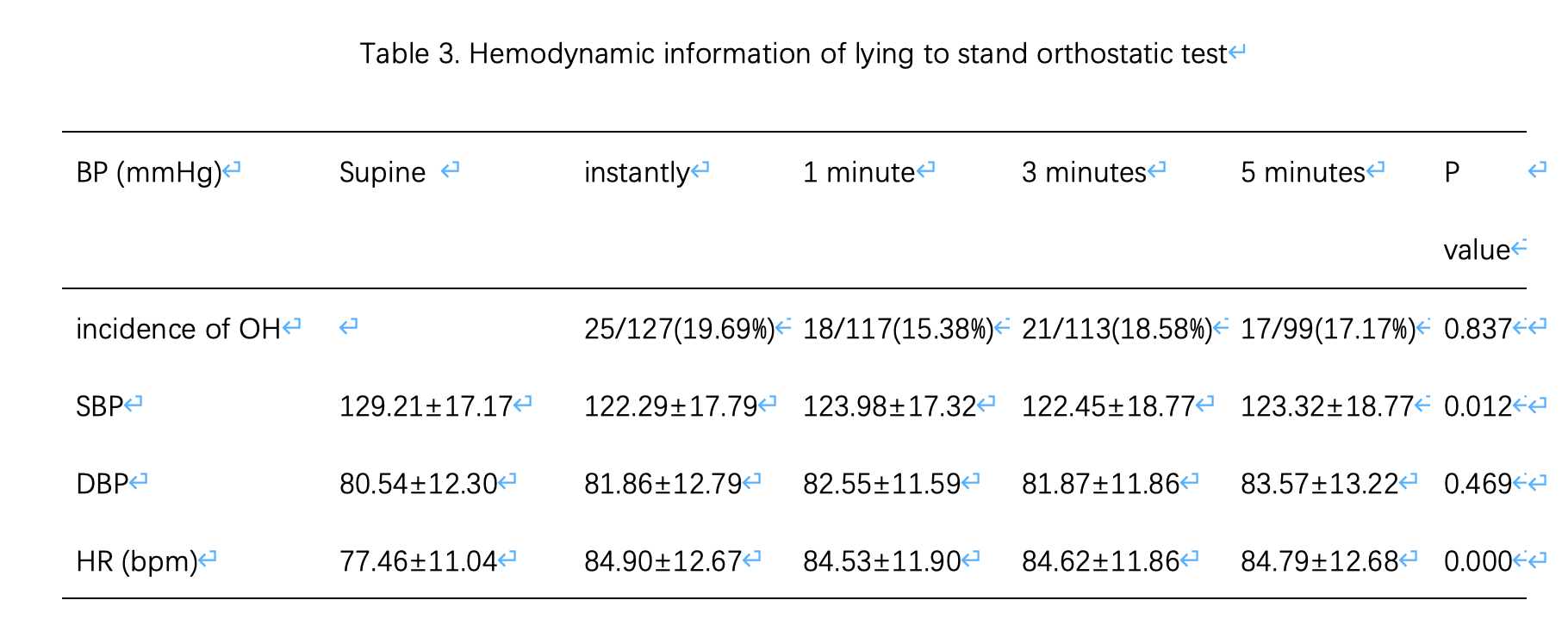
We measured blood pressure (BP) supine and standing up 5 minutes and BP post drug supine and standing up instantly in 132 EOPD. A comprehensive set of clinical features including both motor and non-motor symptoms was assessed, including MDS-UPDRS III, BMI, LEDD, MMSE, MoCA, PDQ-39, MAES, PSQI, RBDSQ and SCOPA-AUT and so on. We compared demographics and clinical characteristics and clinical performance among different orthostatic hypotension diagnosis methods, including OH within 3 minutes, OH within 5 minutes, acute OH post drug, OH within 5 minutes and post drug.
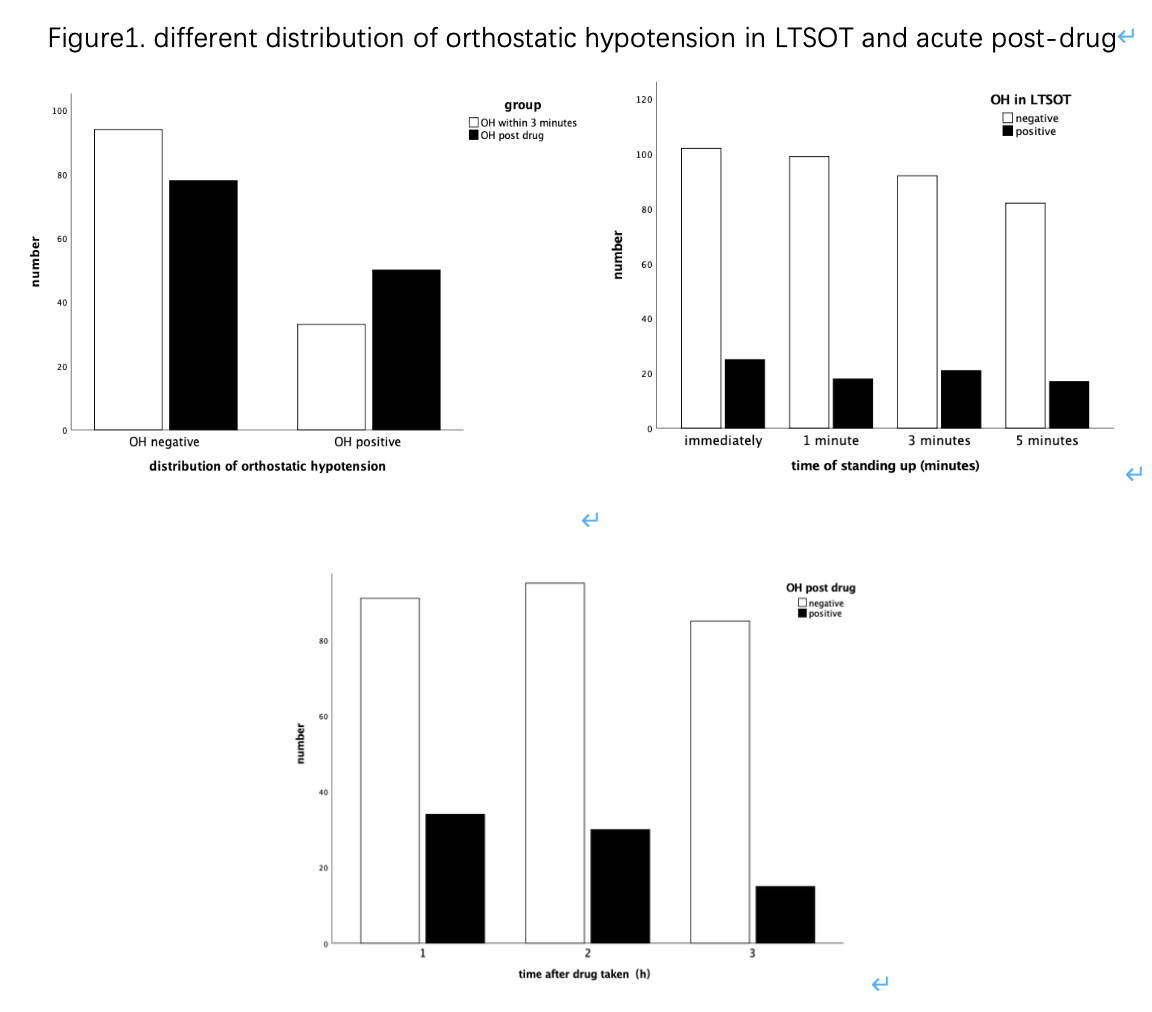
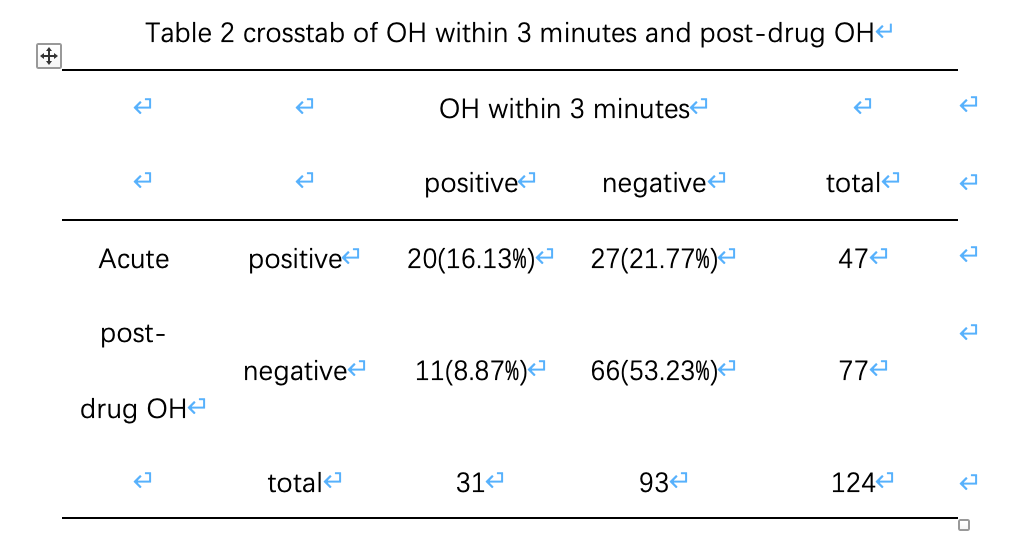
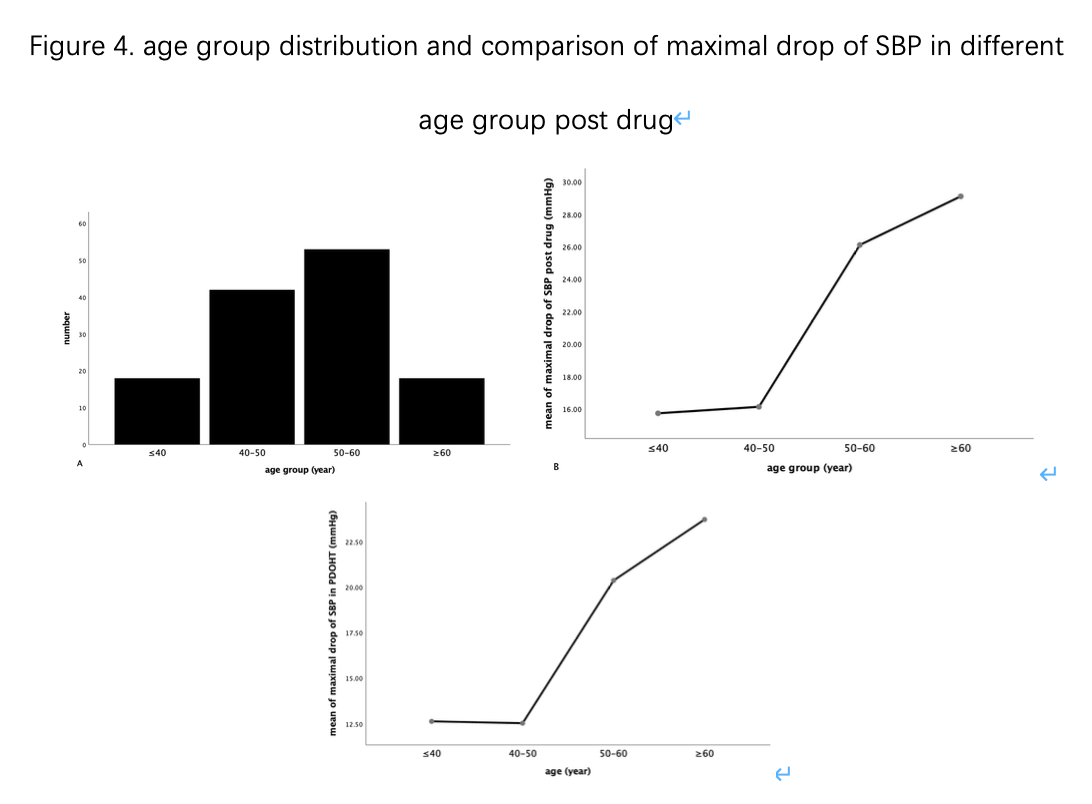
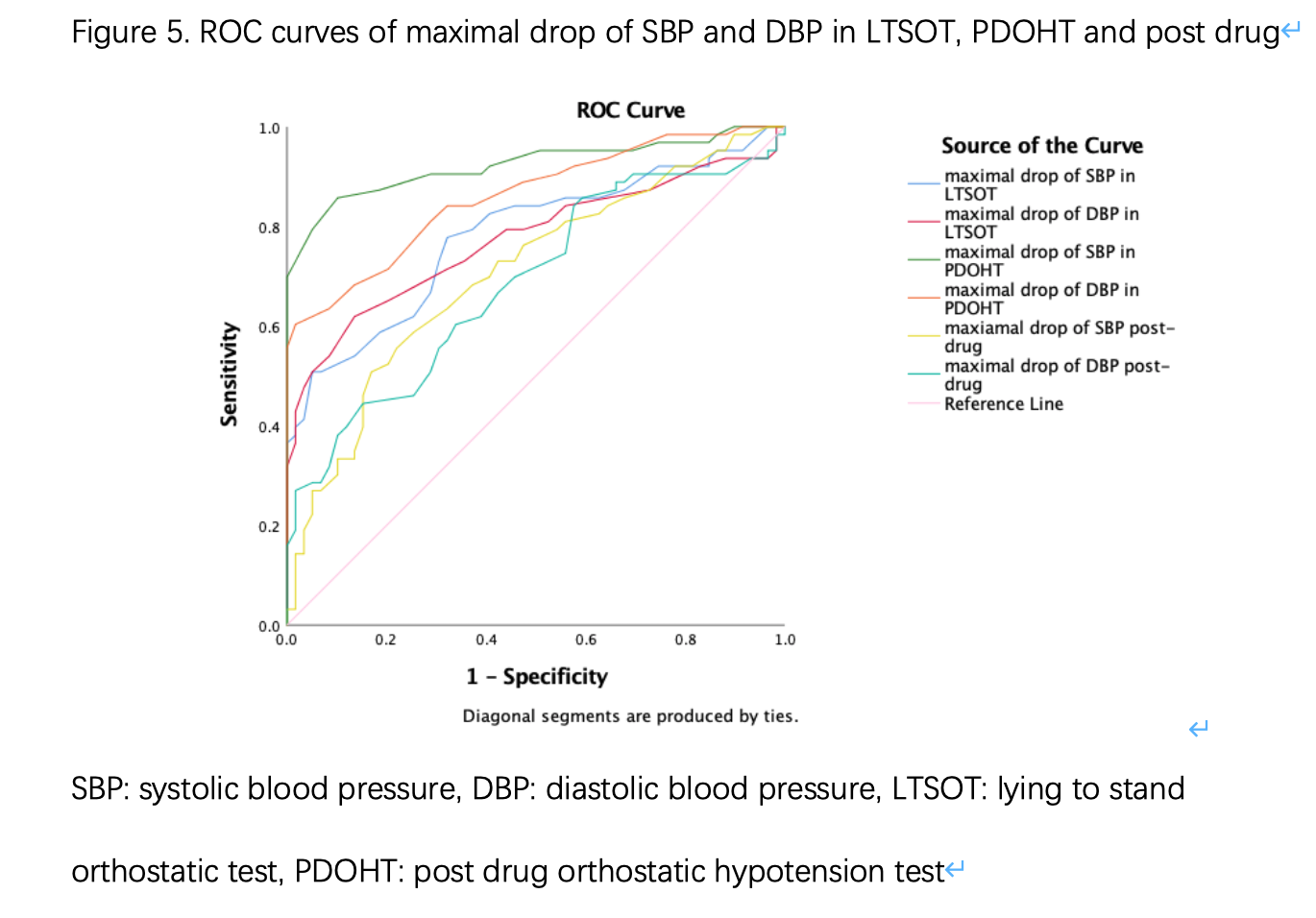
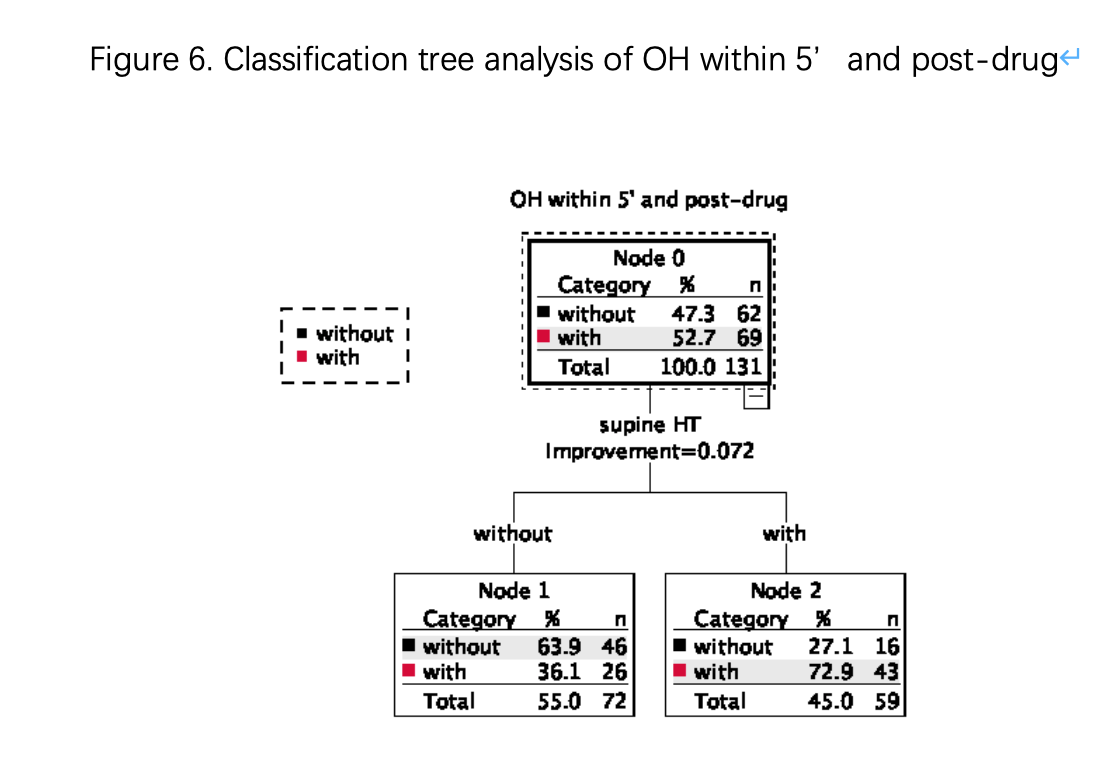
Results: The prevalence of OH within 3 minutes in EOPD was 25.8%, OH within 5 minutes was 36.2%, OH post drug was 39.5%, OH within 5’ and post-drug was 53.0%, difference was statistic significant. 14 patients (11.02%) had OH at the 5th minutes not within the classical 3 min of standing. Maximal drop of SBP in post drug orthostatic test (PDOHT) (P<0.05) in different age groups showed significant difference, especially in elders older than 50 yr whose maximal drop of SBP increased sharply in EOPD. PD patients with OH within 5’ and post-drug performed higher score in constipation, freezing of gait, wearing-off, and better motor response to levodopa. Maximal drop of SBP in PDOHT had the best-combined sensitivity and specificity (area under the ROC curve of 0.923). Risk stratification for OH within 5’and post-drug by means of the classification tree analysis. The subgroup of patients with supine hypertension had a relatively high risk (72.9%) of OH within 5’and post-drug.
Conclusion:
1. delayed OH and OH post-drug was common in EOPD, physician should consider these conditions when diagnose OH in EOPD. 2.supine hypertension was a risk factor for PD patients to be with OH, physician should notice this clinical dilemma to avoid incorrect judgment based on one-time and single-procedure blood pressure or OH test.
To cite this abstract in AMA style:
Z. Liu, D.N Su, J.H Zhou, T. Feng. Orthostatic hypotension in early onset Parkinson’s disease [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/orthostatic-hypotension-in-early-onset-parkinsons-disease/. Accessed February 5, 2026.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/orthostatic-hypotension-in-early-onset-parkinsons-disease/