Category: Parkinson's Disease: Neuroimaging
Objective: The objective of this study was to compare similarities and differences between patient-specific, disease-matched and normative structural connectivity seeding from deep brain stimulation (DBS) electrodes in Parkinson’s disease and retrospective estimation of clinical outcome that they may generate.
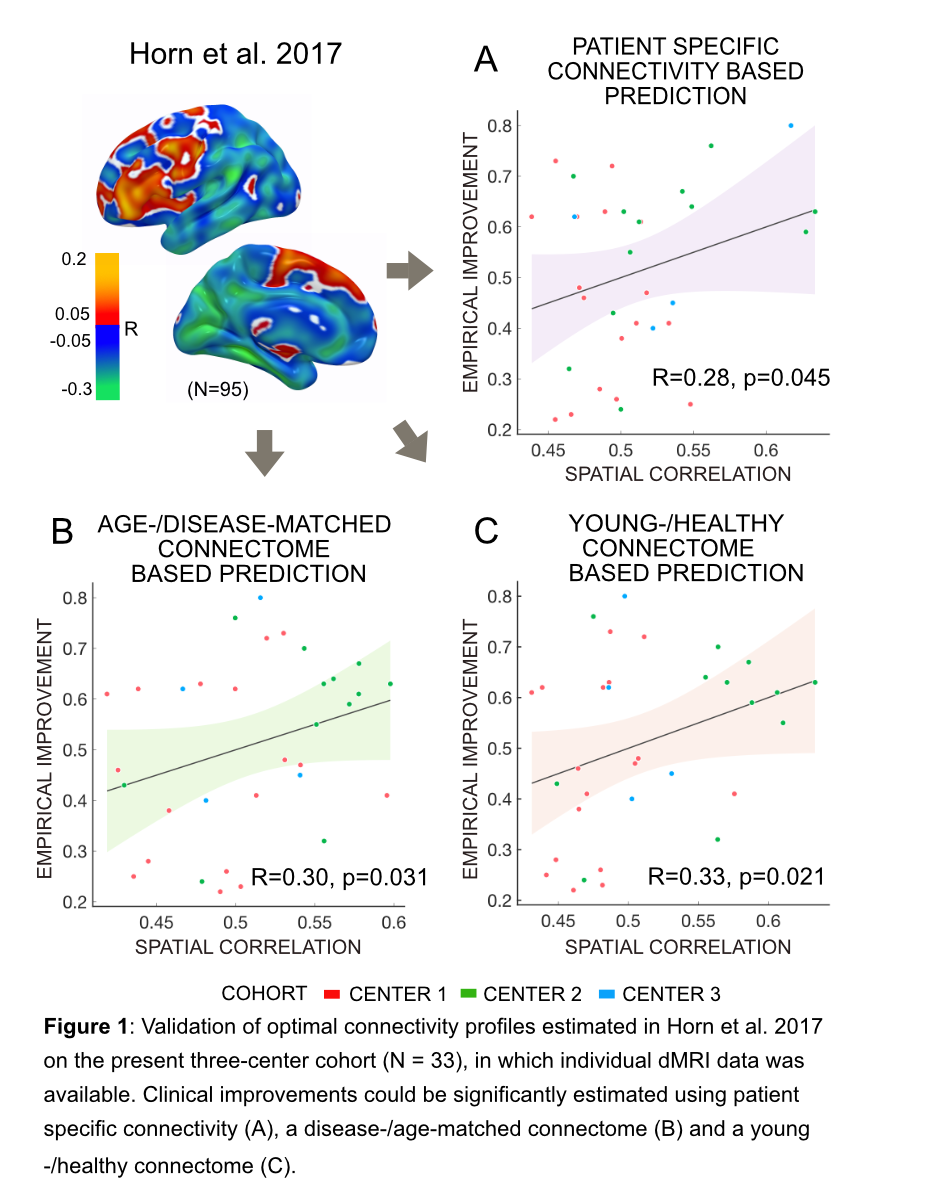
Background: Brain connectivity profiles seeding from DBS electrodes have emerged as informative tools to estimate outcome variability across DBS patients. Given the limitations of acquiring and processing patient-specific diffusion-weighted imaging data, most studies have employed normative atlases of the human connectome [1,2,3,4]. To date, it remains unclear whether patient-specific connectivity information would strengthen the accuracy of such analyses.
Method: Data from 33 patients suffering from PD who underwent surgery at three different centers were retrospectively collected. Stimulation-dependent connectivity profiles seeding from active contacts were estimated using three modalities, namely either patient-specific diffusion-MRI data, disease-matched or normative group connectome data (acquired in healthy young subjects). Based on these profiles, models of optimal connectivity were constructed and used to retrospectively estimate the clinical improvement in out of sample data.
Results: All three modalities resulted in highly similar optimal connectivity profiles that could largely reproduce findings from prior research based on a novel multi-center cohort [Figure1]. However, in a data-driven approach that estimated optimal whole-brain connectivity profiles, out-of-sample estimation of clinical improvements were made and ranged within a similar magnitude when applying either of the three modalities (R = 0.43 at p = 0.001 for patient-specific connectivity; R = 0.25, p = 0.048 for the age- and disease-matched group connectome; R = 0.31 at p = 0.028 for healthy-/young connectome).[Figure2]
Conclusion: The use of patient-specific connectivity and normative connectomes lead to identical main conclusions about which brain areas are associated with clinical improvement. Still, although results were not significantly different, they hint at the fact that patient-specific connectivity may bear the potential of estimating slightly more variance when compared to group connectomes. Our findings further support the role of DBS electrode connectivity profiles as a promising method to guide surgical targeting and DBS programming.
References: [1] Horn, A., Reich, M., Vorwerk, J., Li, N., Wenzel, G., Fang, Q., Schmitz-Hübsch, T., Nickl, R., Kupsch, A., Volkmann, J., Kühn, A.A., Fox, M.D., 2017b. Connectivity Predicts deep brain stimulation outcome in Parkinson disease. Ann. Neurol. 82, 67–78. [2] Horn, A., 2019. The impact of modern-day neuroimaging on the field of deep brain stimulation. Curr. Opin. Neurol. 32, 511–520.
To cite this abstract in AMA style:
Q. Wang, H. Akram, M. Muthuraman, G. Gonzalez-Escamilla, S. A. Sheth, G. Groppa, N. Vanegas-Arroyave, L. Zrinzo, N. Li, A. Kühn, A. Horn. Normative vs. patient-specific brain connectivity in Deep Brain Stimulation [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/normative-vs-patient-specific-brain-connectivity-in-deep-brain-stimulation/. Accessed December 23, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/normative-vs-patient-specific-brain-connectivity-in-deep-brain-stimulation/