Category: Parkinson's Disease: Neuroimaging
Objective: To investigate the relationship between brain ventricular and gray matter volumes and objective balance and gait metrics in people with Parkinson’s disease (PD).
Background: Instrumented measures of mobility are more sensitive to decline in mobility than standard clinical measures and no prior studies have used instrumented measures of mobility to examine how axial symptoms in PD patients were affected by ventricular dilatation or grey matter volume. In this study, we aimed to determine which domains of balance and gait were related to ventricular, subcortical grey, and cortical grey matter volumes.
Method: 90 people with idiopathic PD and 50 age-matched control (HC) subjects (PD mean (SD) age 68.5 (8.0) years, MDS-UPDRS-III 39.7 (11.7) off medication) were recruited. MRI data were acquired using 3.0T Siemens scanner and processed using HCP pipeline [1]. Volume outputs from the pipeline were normalized by intracranial volume and age. The total ventricular volume is the sum of lateral, third and fourth ventricle volumes. Wearable inertial sensors quantified the following domains of gait and balance: spatiotemporal gait, anticipatory postural adjustments (APA), automatic postural responses (APR), and standing postural sway measured on foam surface with eyes open. Pearson correlation correlated the age-controlled balance/gait metrics with brain volume metrics. ANCOVA tested differences in slope between PD and HC. FDR method was used to correct for multiple comparisons.
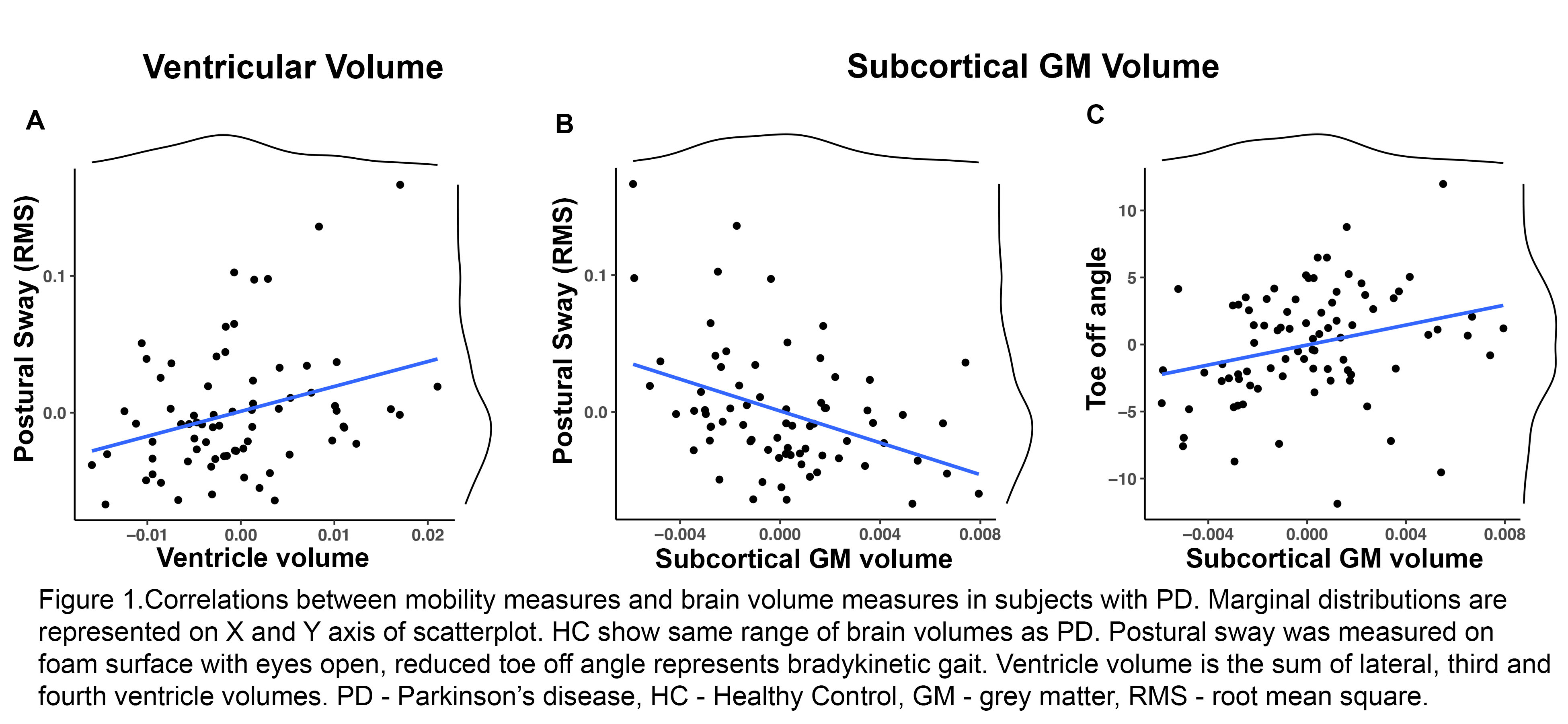
Results: Ventricular volume was positively correlated with root mean square (RMS) of standing postural sway (R=0.3, p=0.02) in PD as shown in figure1A. Likewise, subcortical grey matter volume was negatively correlated with RMS of standing postural sway (R=-0.39, p=0.002) [figure1B] and was also positively correlated with gait domain – foot angle at toe off (R=0.29, p=0.01) [figure1C]. Ventricular volume was also positively correlated with Postural Instability and Gait Disability score (PIGD, R=0.34, p=0.001) and negatively correlated with the Activity Specific Balance Confidence Scale (ABC; R=-0.26, p=0.01). ANCOVA results show significant effect of brain volumes and diagnosis on balance/gait metrics, but no significant interaction.
Conclusion: Our findings suggest that increased brain ventricular volume and reduction in subcortical volume is associated with standing balance dysfunction and a bradykinetic gait pattern in people with PD.
References: 1. Glasser, M. F., Sotiropoulos, S. N., Wilson, J. A., Coalson, T. S., Fischl, B., Andersson, J. L., … & Van Essen, D. C. (2013). The minimal preprocessing pipelines for the Human Connectome Project. Neuroimage, 80, 105-124.
To cite this abstract in AMA style:
A. Ragothaman, A. Giritharan, M. Mancini, O. Miranda-Dominguez, D. Fair, J. Nutt, F. Horak. Association Between Ventricle/Brain Volumes and Mobility Metrics in Parkinson’s Disease [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/association-between-ventricle-brain-volumes-and-mobility-metrics-in-parkinsons-disease/. Accessed January 1, 2026.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/association-between-ventricle-brain-volumes-and-mobility-metrics-in-parkinsons-disease/