Category: Parkinson's Disease: Neuroimaging
Objective: To investigate neural correlates associated with olfactory dysfunction using fMRI and EEG in Parkinsonism.
Background: Patients with Parkinsonism experience non-motor symptoms during the onset and progress of disease. Hyposmia may be a characteristic sign of Parkinson’s disease (PD), as revealed by electrophysiological studies, with over 95% patients with significant olfactory loss [1-2].
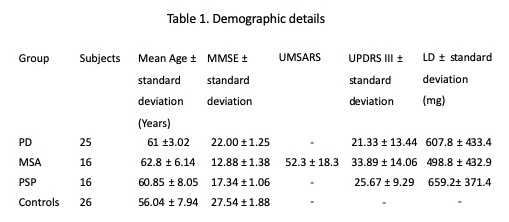
Method: All right handed PD (25), MSA (16) and PSP (16) patients (Table 1) were recruited from the movement disorder clinics of our institute. Standard diagnostic and exclusion criteria were followed. MR studies were carried out in a 3T MR scanner using 32 channel head coils (M/s. Philips, the Netherlands) in the “on” state. Echo planar imaging sequence was used for functional MRI studies using a block design. The patients underwent sniff kit (Burghart Messtechnik GmbH, Germany) test during the active state and a period of rest (no smell) during the baseline state. Data was analysed using SPM12 and EEG lab [3-4]. Two sample t-test (p<0.05, cluster threshold 10) was used for group analysis. Spearman correlation analysis was done by using STATA (ver. 12) for testing level of significance. Multiple comparisons was done using Bonferroni post-hoc test, Kruskal-wallis test.
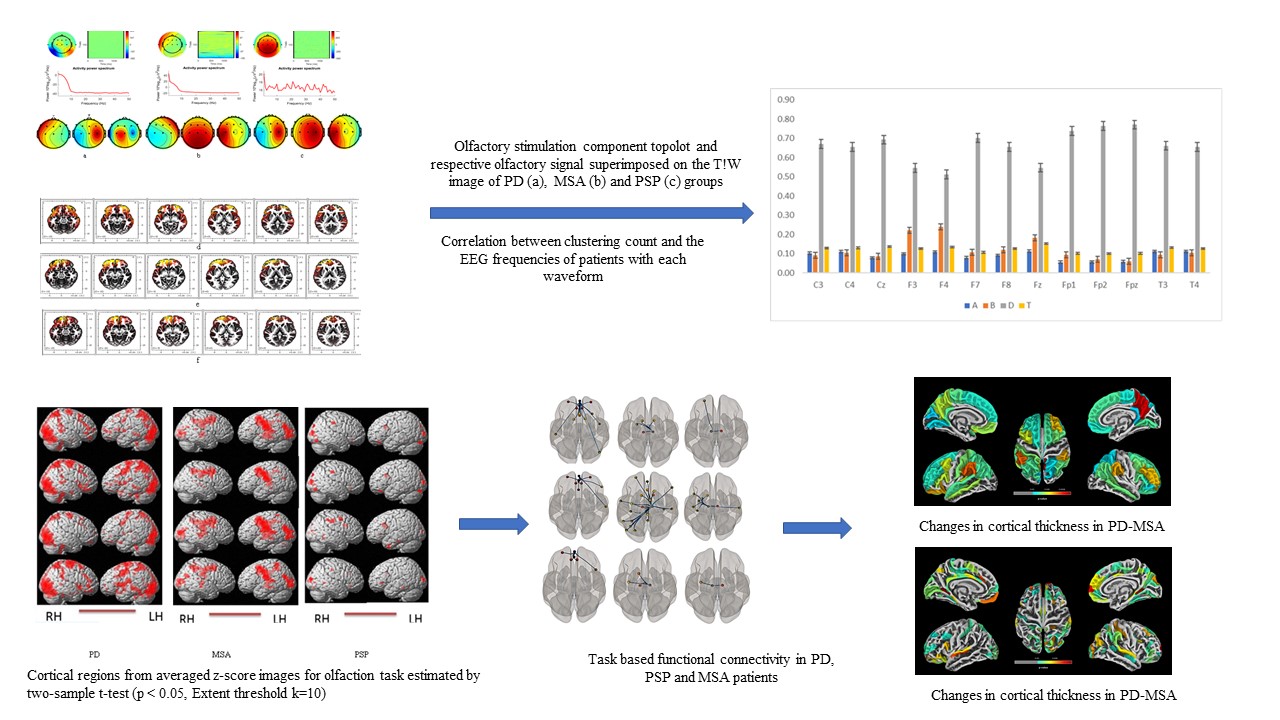
Results: All patient groups had less activation in olfaction areas (Parkinson’s disease < MSA < PSP). Activation was absent in middle frontal, orbitofrontal, and temporal cortex, inferior frontal, insular, and cingulate cortex in patients with Parkinson’s disease (Figure 1). In patients with MSA and PSP, activation was observed in bilateral middle frontal, orbito-frontal cortex; left hemispheric inferior frontal, temporal, and cingulate cortex areas [3]. EEG revealed a similar pattern on frequency change of Delta waveform in PD and MSA groups, but PSP exhibited different pattern in the alpha waveform. Alteration in the spectral powers (increases in delta and theta; decrease in alpha and beta; less significant in gamma) in PD and MSA patients for smell detection and identification revealed a similar trend, and was different in PSP group.
Conclusion: Differential brain activation pattern was observed in PD, MSA and PSP during hyposmia task. EEG exhibited different frequency of spectral power delta and alpha waves and a positive correlation with the clinical score in the frontal cortex suggesting its role in the signal transmission to temporal and cingulate regions.
References: 1. Iannilli E Stephan L, Hummel T, Reichmann H, Haehner A. 2017. Olfactory impairment in Parkinson’s disease is a consequence of central nervous system decline. J Neurol. 264:1236-1246 2. 2. Haehner A, Hummel T, Reichmann H. 2009. Olfactory dysfunction as a diagnostic marker for Parkinson’s disease. Expert Rev Neurother. 912:1773-9 3. 3. Friston KJ 2003. Learning and inference in the brain. Neural Netw.16:1325–52 4. 4. Delorme A, Makeig S 2004. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics. Journal of Neuroscience Methods. 134:9-21.
To cite this abstract in AMA style:
S. Kumaran, A. Ankeeta, S. Chaudhary, P. Bhat, V. Goyal. Hyposmia as a biomarker in patients with Parkinson’s disease and atypical Parkinsonism [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/hyposmia-as-a-biomarker-in-patients-with-parkinsons-disease-and-atypical-parkinsonism/. Accessed April 3, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/hyposmia-as-a-biomarker-in-patients-with-parkinsons-disease-and-atypical-parkinsonism/