Session Information
Date: Wednesday, September 25, 2019
Session Title: Neuroimaging
Session Time: 1:15pm-2:45pm
Location: Les Muses Terrace, Level 3
Objective: To determine the clinical and imaging correlates of impaired cerebral autoregulation as measured with cerebral vasoreactivity (CVR) in patients with idiopathic Parkinson’s disease (PD).
Background: Contribution of subclinical cerebrovascular disease (CVD) on Parkinson’s disease remains controversial. Impaired cerebral autoregulation (loss of cerebral vasoreactivity), and leukoaraioisis (white matter damage) represent non-invasive markers of CVD, which have been reported in PD patients to increase mortality[1, 2]; yet their impact on severity remains unknown[3]; Thus, we designed a study to assess CVR and its clinical and imaging correlates in a cohort of PD patients.
Method: Consecutive patients with PD diagnosis underwent transcranial Doppler Ultrasound (temporal bone window) was performed in ON state, and mean blood flow velocity (cm/s) was recorded before and after stimulus with 7% carbon dioxide inhalation during 5-minutes. Impaired CVR was defined as a difference less than 5% after hypercapnic stimulus [4]. Leukoaraiosis was evaluated with Fazekas scale. We excluded those with history of CVD (stroke or transient ischemic attack).
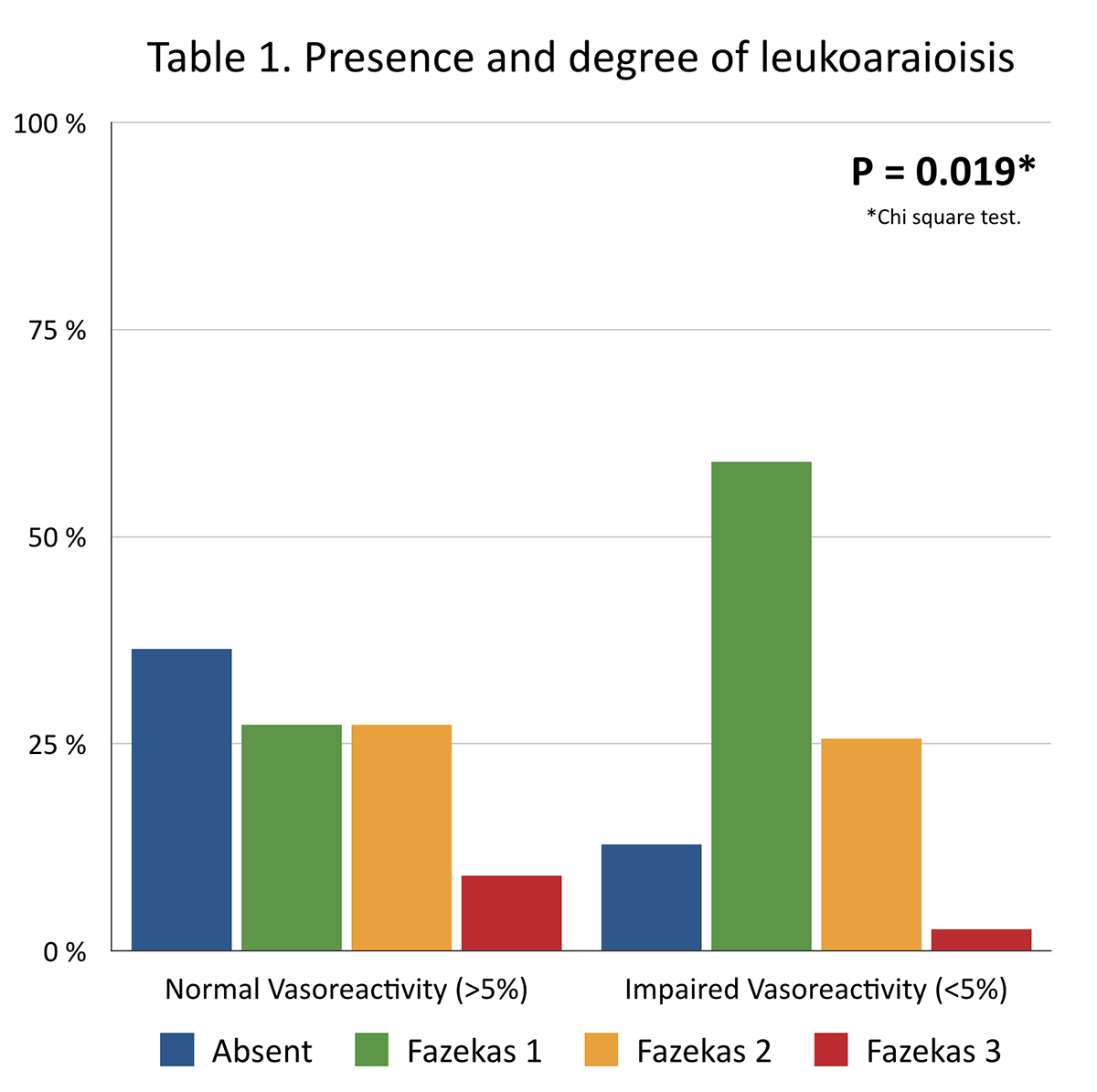
Results: 72 patients were included, and impaired CVR was found in 39 (54.2%), when comparing variables between groups, we found that patients with impaired CVR had a higher proportion of non-tremor dominant phenotype at onset (56.4% vs 27.3%; p=0.013), and were receiving significantly higher levodopa equivalent daily doses (965.9±610.6mg vs. 689.3±383.1, p=0.025), without difference in disease duration, or severity. Patients with impaired CVR had a significantly higher prevalence of white matter changes (Figure 1).
Conclusion: In PD patients, impairment of cerebral vasoreactivity is highly prevalent and associated with of white matter changes (but not severity), and higher levodopa doses, albeit unrelated to disease severity or duration.
References: 1. Rektor I, Goldemund D, Bednarik P, Sheardova K, Michalkova Z, Telecka S, et al. Impairment of brain vessels may contribute to mortality in patients with Parkinson’s disease. Mov Disord. 2012;27(9):1169-72. 2. Malek N, Lawton MA, Swallow DM, Grosset KA, Marrinan SL, Bajaj N, et al. Vascular disease and vascular risk factors in relation to motor features and cognition in early Parkinson’s disease. Mov Disord. 2016;31(10):1518-26. 3. Song IU, Lee JE, Kwon DY, Park JH, Ma HI. Parkinson’s disease might increase the risk of cerebral ischemic lesions. Int J Med Sci. 2017;14(4):319-22. 4. Zamani B, Mehrabani M, Fereshtehnejad SM, Rohani M. Evaluation of cerebral vasomotor reactivity in Parkinson’s disease: is there any association with orthostatic hypotension? Clin Neurol Neurosurg. 2011;113(5):368-72.
To cite this abstract in AMA style:
I. Estrada-Bellmann, D. Cantú-García, S. Castillo-Torres, A. Mendoza-García, H. Sánchez-Terán, D. Díaz-Pérez, D. Roque-Martínez, S. Saldívar-Dávila, H. Martínez, T. Moreno-Andrade, B. Chávez-Luévanos, F. Góngora-Rivera. Impaired cerebral vasoreactivity in patients with Parkinson’s disease: clinical and imaging correlates [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/impaired-cerebral-vasoreactivity-in-patients-with-parkinsons-disease-clinical-and-imaging-correlates/. Accessed November 17, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/impaired-cerebral-vasoreactivity-in-patients-with-parkinsons-disease-clinical-and-imaging-correlates/