Session Information
Date: Wednesday, September 25, 2019
Session Title: Neuroimaging
Session Time: 1:15pm-2:45pm
Location: Les Muses Terrace, Level 3
Objective: To evaluate the association between Mild Behavioral Impairment (MBI) and pattern of brain activity during a set-shifting task in Parkinson’s disease (PD).
Background: MBI is a neurobehavioral syndrome characterized by later life emergence of sustained neuropsychiatric symptoms (NPS), as an at-risk state for incident cognitive decline and dementia [1]. Prior studies have been reported that NPS have a negative impact on cognitive abilities in PD patients [2], and we have recently revealed a strong correlation between MBI and cognitive performance [3]. However, the underlying neural activity patterns linked to MBI in PD are unknown.
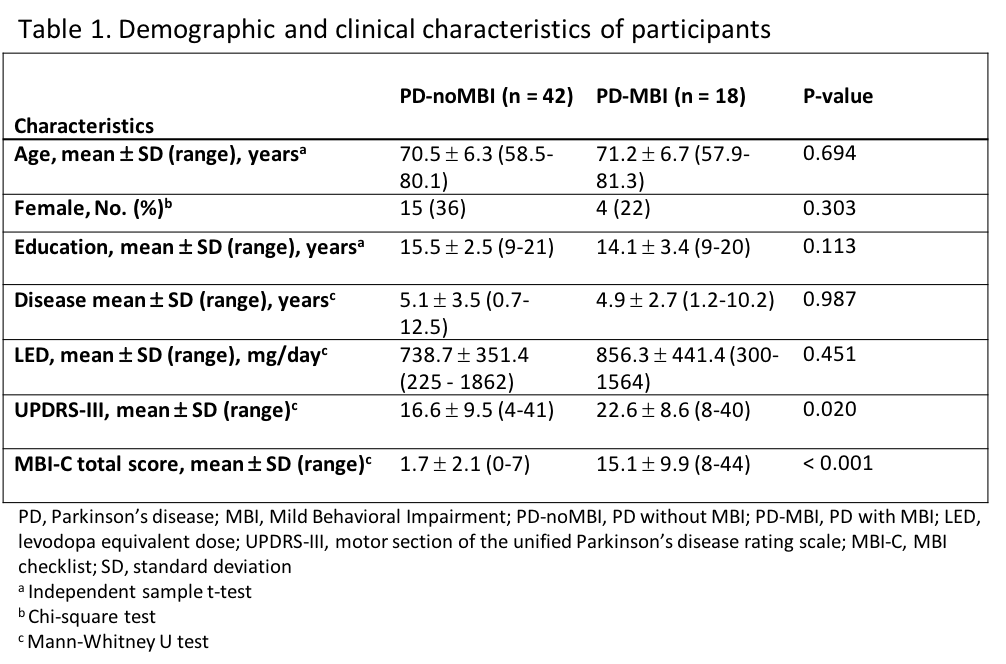
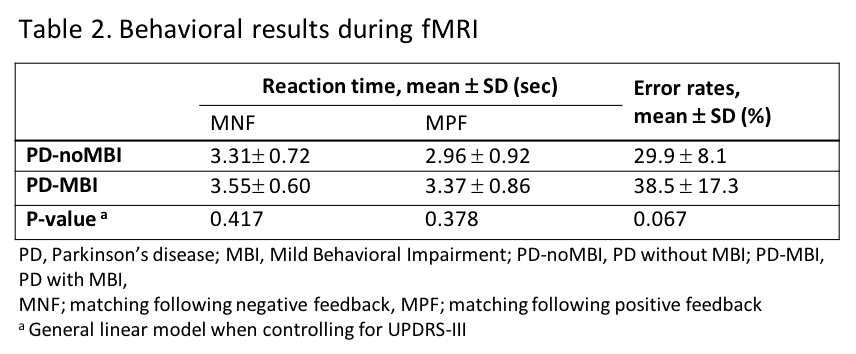
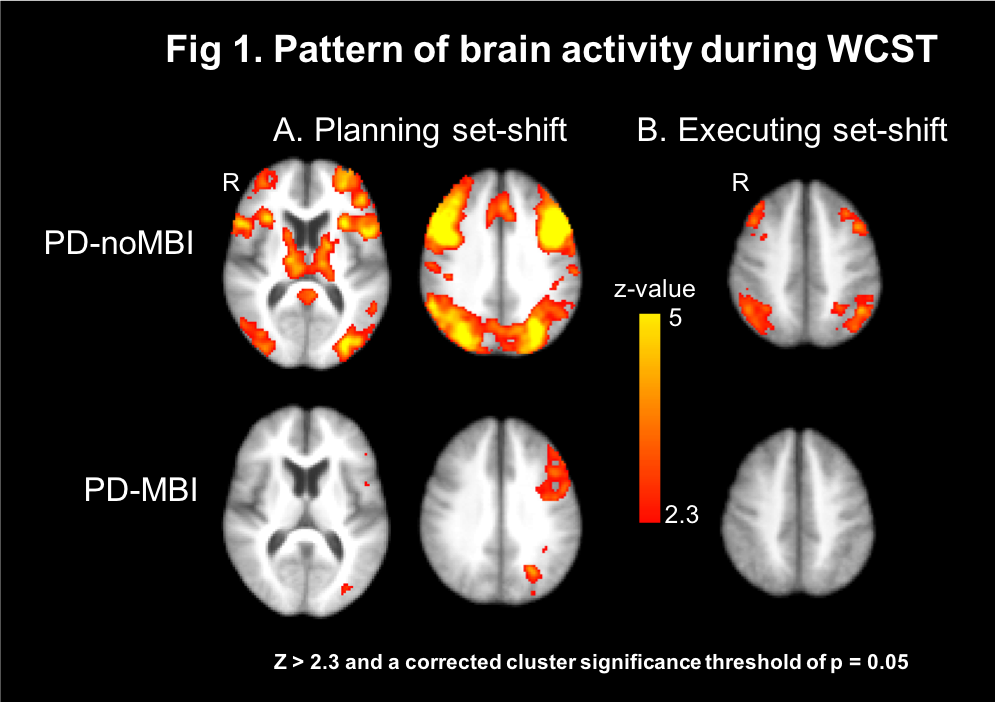
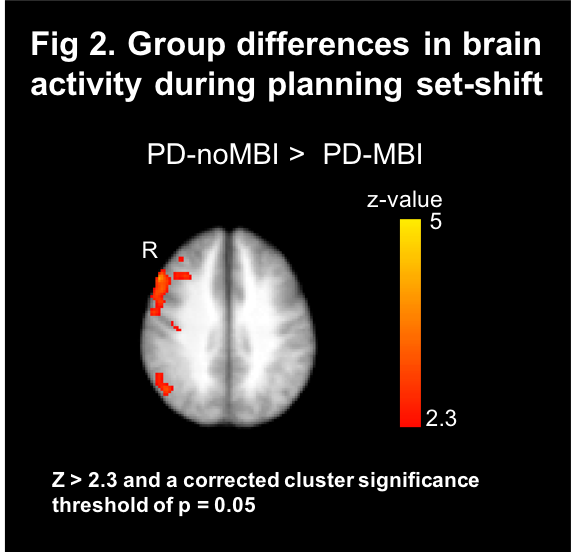
Method: Sixty non-demented PD patients were scanned by fMRI during performance of the Wisconsin Card Sorting Task (WCST). MBI was evaluated using MBI-checklist (MBI-C) [4], and PD patients were divided into two groups, PD-MBI and PD-noMBI, based on the cut-point of 7.5 [5,6]. For fMRI data, two contrasts were computed, receiving negative feedback vs. receiving positive feedback (planning a set-shift) and matching following negative feedback vs. matching following positive feedback (executing a set-shift) [7].
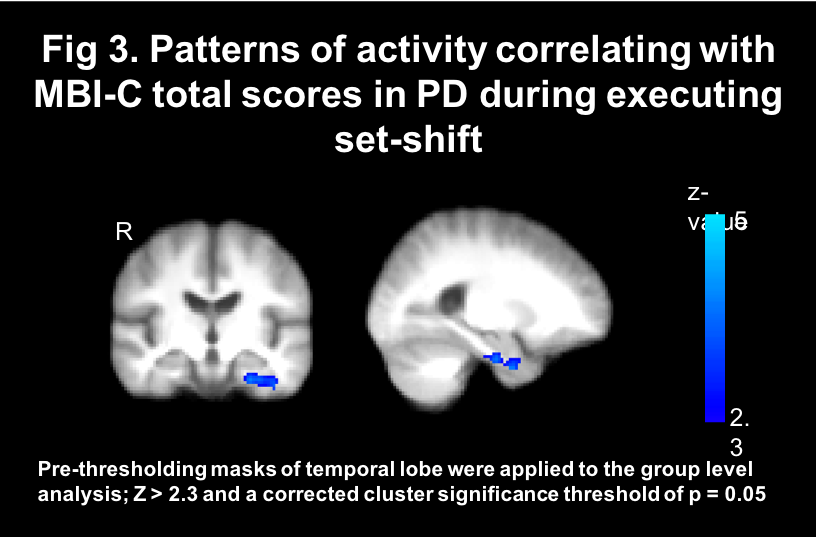
Results: Among 60 PD patients, 18 were categorized as PD-MBI [table1]. There were no group differences in mean reaction times and error rates for the WCST [table2]. During planning a set-shift, PD-noMBI showed significant activity in the prefrontal, parietal and lateral occipital areas, caudate nucleus, and thalamus bilaterally. However, PD-MBI showed significant activation only in left prefrontal and lateral occipital area. During executing a set-shift, PD-noMBI revealed significant activation in the bilateral frontal and parietal area, but PD-MBI had no significant activation [figure1]. In group comparisons, PD-MBI revealed less activity in the right frontoparietal area while planning a set-shift compared to PD-noMBI [figure2]. While executing a set-shift, there was no group difference in brain activity, but we found negative correlations of MBI-C total scores with the left parahippocampal cortex activity in the all PD patients [figure3].
Conclusion: We found that MBI is associated with deficiency of activation in the frontoparietal and the medial temporal regions during cognitive set-shift task. These results suggest that MBI affects posterior cortical circuits that has been associated with a faster rate of progression to dementia [8] as well as executive impairment in PD.
References: 1. Ismail Z, Smith EE, Geda Y, et al. Neuropsychiatric symptoms as early manifestations of emergent dementia: Provisional diagnostic criteria for mild behavioral impairment. Alzheimers Dement. 2016;12(2):195-202. 2. Hanganu A, Monchi O. Interaction Between Neuropsychiatric Symptoms and Cognitive Performance in Parkinson’s Disease: What Do Clinical and Neuroimaging Studies Tell Us? Curr Neurol Neurosci Rep 2018;18:91 3. Yoon EJ, Ismail Z, Hanganu A, Kibreab M, Hammer T, Cheetham J, Kathol I, Sarna J, Martino D, Furtado S, Monchi O. Mild Behavioral Impairment is linked to worse cognition and brain atrophy in Parkinson’s disease. Neurology. In revision. 4. Ismail Z, Aguera-Ortiz L, Brodaty H, et al. The Mild Behavioral Impairment Checklist (MBI-C): A Rating Scale for Neuropsychiatric Symptoms in Pre-Dementia Populations. J Alzheimers Dis 2017;56:929-938. 5. Mallo SC, Ismail Z, Pereiro AX, et al. Assessing mild behavioral impairment with the mild behavioral impairment checklist in people with subjective cognitive decline. Int Psychogeriatr 2018:1-9. 6. Mallo SC, Ismail Z, Pereiro AX, et al. Assessing Mild Behavioral Impairment with the Mild Behavioral Impairment-Checklist in People with Mild Cognitive Impairment. J Alzheimers Dis 2018;66:83-95. 7. Monchi O, Petrides M, Petre V, Worsley K, Dagher A. Wisconsin Card Sorting Revisited: Distinct Neural Circuits Participating in Different Stages of the Task Identified by Event-Related Functional Magnetic Resonance Imaging. J Neurosci 2001 ;21(19) :7733-7741. 8. Williams-Gray CH, Evans JR, Goris A, et al. The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the CamPaIGN cohort. Brain 2009;132:2958-2969.
To cite this abstract in AMA style:
EJ. Yoon, Z. Ismail, M. Kibreab, T. Hammer, J. Cheetham, I. Kathol, M. Ramezani, S. Lang, J. Sarna, D. Martino, S. Furtado, O. Monchi. Patterns of brain activity linked to Mild Behavioral Impairment in Parkinson’s disease [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/patterns-of-brain-activity-linked-to-mild-behavioral-impairment-in-parkinsons-disease/. Accessed December 23, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/patterns-of-brain-activity-linked-to-mild-behavioral-impairment-in-parkinsons-disease/