Session Information
Date: Wednesday, September 25, 2019
Session Title: Neuroimaging
Session Time: 1:15pm-2:45pm
Location: Les Muses Terrace, Level 3
Objective: We describe our series of patients with iron deposition in basal ganglia (IDBG) and hypothesize differences regarding the affected nuclei in patients with movement disorders (MD).
Background: IDBG has been associated both with normal aging and neurodegenerative disorders such as parkinsonian syndromes [1]. In this context, it remains unclear whether it implies a pathological significance when found in neuroimaging studies arranged in routine medical practice [2, 3, 4]
Method: We designed a retrospective cross-sectional study including patients with IDBG evidenced in magnetic resonance imaging (MRI) along a fifteen years’ period in a tertiary care center.
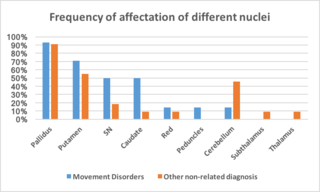
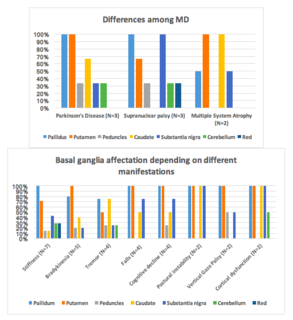
Results: Twenty-five patients were reported to present IDBG in MRI. Fifty-six per cent was diagnosed with entities within the spectrum of MD (Parkinson’s disease and progressive supranuclear palsy as most frequent, 21,4 % each), whereas 44 % had non-MD diagnosis (stroke as most frequent, 36,4 %) [figure 1]. Mean age was similar in both groups (67,7 and 66,7 years respectively). Caudate nucleus was significantly more affected among patients with MD (p=0,04) and similar non-significant trends were observed for putamen and substantia nigra. Pallidus was similarly affected in both groups [figure 2]. Each MD diagnosis and specific clinical manifestations at first consultation were correlated with a particular pattern of affected basal ganglia [figure 3], being consistent with the reviewed literature.
Conclusion: Incidental IDBD could have different patterns of nuclei involvement in MD vs non MD patients, as our series illustrates. Pathological significance of IDBG still remains unclear and further investigation is needed in order to clarify neuroimaging criteria and its clinical implications.
References: 1.- Berg D, Hochstrasser H. Iron metabolism in Parkinsonian syndromes. Mov Disord. 2006 Sep;21(9):1299-310. 2.- Rossi M, Ruottinen H, Soimakallio S, Elovaara I, Dastidar P. Clinical MRI for iron detection in Parkinson’s disease. Clin Imaging. 2013 Jul-Aug;37(4):631-6. 3.- Hingwala DR, Kesavadas C, Thomas B, Kapilamoorthy TR. Susceptibility weighted imaging in the evaluation of movement disorders. Clin Radiol. 2013 Jun;68(6):e338-48. 4.- Graham JM, Paley MN, Grünewald RA, Hoggard N, Griffiths PD. Brain iron deposition in Parkinson’s disease imaged using the PRIME magnetic resonance sequence. Brain 2000 Dec;123 Pt 12:2423-31.
To cite this abstract in AMA style:
á. Beltrán Corbellini, P. Pérez Torre, A. Alonso Cánovas, F. Rodríguez Jorge, JL. Chico García, P. Parra Díaz, E. Natera Villalba, A. Gómez López, S. Fanjul Arbos, JL. López Sendón, JC. Martínez Castrillo, I. Parées Moreno. Incidental iron deposition in basal ganglia: does the pattern matter? Fifteen years’ experience in a tertiary care center. [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/incidental-iron-deposition-in-basal-ganglia-does-the-pattern-matter-fifteen-years-experience-in-a-tertiary-care-center/. Accessed October 22, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/incidental-iron-deposition-in-basal-ganglia-does-the-pattern-matter-fifteen-years-experience-in-a-tertiary-care-center/